The vitamin D-ilemma Part 5
How can you get enough vitamin D if you don't want to take supplements?
Part 5: Optimising your vitamin D status
In Part 4 of this miniseries on vitamin D, I delved into the evidence that the link between low vitamin D (more precisely, 25-hydroxyvitamin D) status and a host of chronic diseases, is one of reverse causation - that is, low serum levels of 25-hydroxyvitamin D may be the result of certain disease processes such as inflammation and chronic intracellular infection, rather than their cause.
Nonetheless, given that the biologically-active form of (so-called) vitamin D - the secosteroid hormone calcitriol - is integrally involved in controlling the expression of thousands of genes which regulate a vast array of processes that are vital to health and healing, it makes sense to take steps to optimise its activity. Let's break that down into getting enough of the precursors, which I'll cover in this part of the miniseries, and optimising activation of the precursors into calcitriol and optimising vitamin D receptor function which I'll discuss in the next part (yes, I know I told you in Part 4 that this would be my last instalment of the series, but I keep on finding more fascinating research that I want to share with you!).
How to get enough vitamin D if you don't want to take supplements
Safe sunbathing
Exposure to sunlight has benefits that extend far beyond the generation of 7-dehydrocholesterol (the precursor to cholecalciferol, or vitamin D3) in our skin:
"A substantial body of evidence shows that sunlight has health benefits and that these are independent of vitamin D and thus cannot be reproduced by oral supplementation."
Sunlight Has Cardiovascular Benefits Independently of Vitamin D
Every wavelength of light in full-spectrum sunlight that reaches the Earth's surface, from 280 nanometre wavelength ultraviolet B (UVB) to 2500 nm near-infrared (NIR), has specific biological effects.
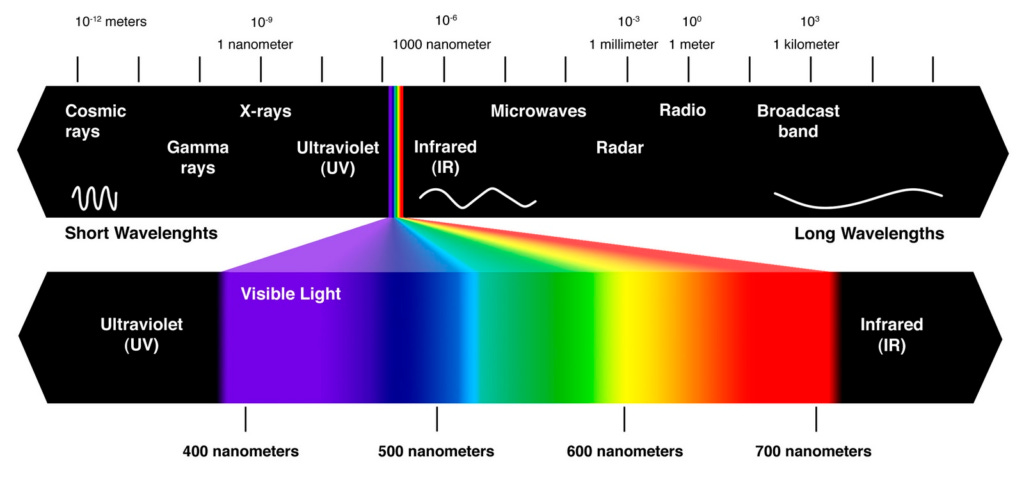
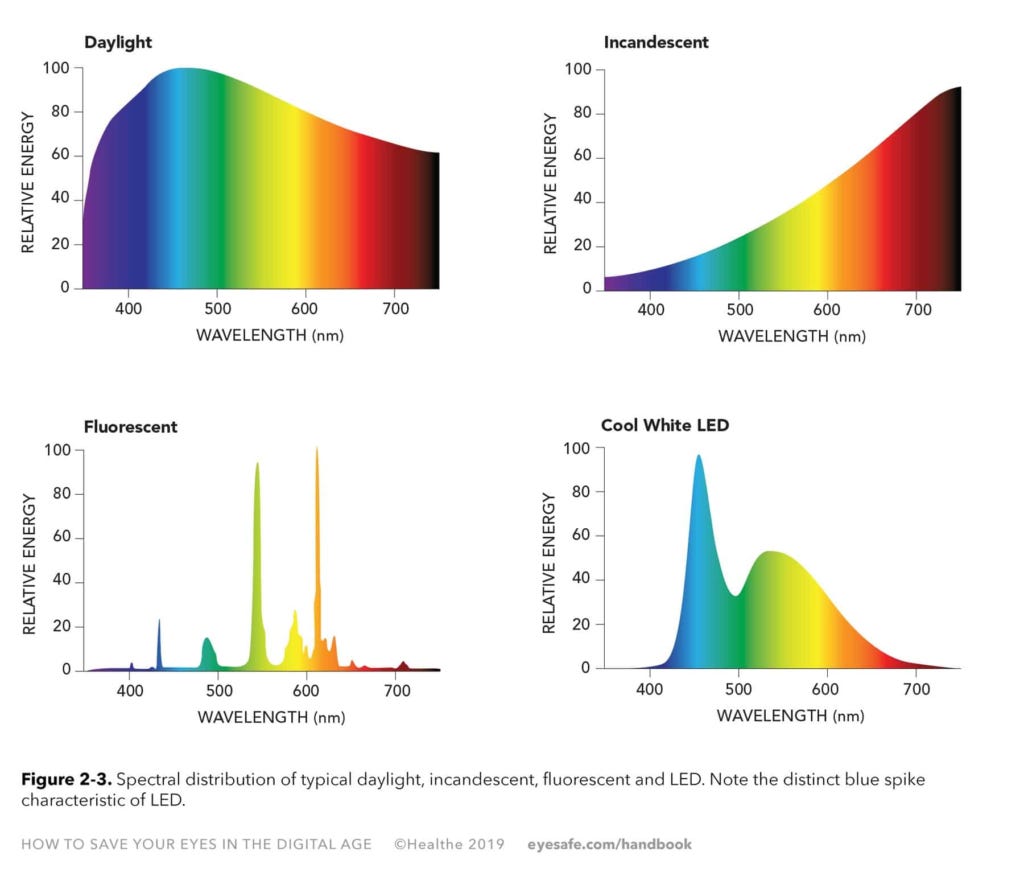
Just as we suffer adverse health consequences from eating a nutritionally unbalanced diet (too much of some macro- and micronutrients, not enough of others), our health suffers from an unbalanced light diet (too much of some wavelengths, not enough of others) due to spending most of our days indoors, under various forms of artificial lighting1.
The specific wavelengths that stimulate the production of cholecalciferol from 7-dehydrocholesterol in the microvessels of the skin, fall within the UVB spectrum. As you might remember from Part 1, upwards of 99 per cent of UVB radiation emitted by the sun is absorbed by the stratospheric ozone layer before it ever reaches the earth’s surface, and the sun must be at least 45 degrees above the horizon for sufficient UVB to penetrate the atmosphere in order to stimulate cholecalciferol synthesis.
To safely meet your biological requirement for UVB while avoiding sunburn, you should start exposing your bare skin to sunlight for brief periods - just a couple of minutes per day - commencing in the spring, and covering up or seeking shade as soon as your skin turns very slightly pink or begins to blanch (i.e. remains pale for a brief period of time after you firmly press the skin of your upper arm, and then release the pressure). Extend the period of exposure until you reach the appropriate 'dose' of sunlight for your skin type. Fair-skinned people need only 4-9 minutes (depending on latitude) of midday summer sun, to produce the equivalent of a 1000 IU oral dose of cholecalciferol. But at a latitude of 62.5° N, those with the darkest skin type would need 36 minutes of that same midday summer sun to make the same amount of vitamin D3.
The D-Minder app allows you to input your location and skin type in order to identify the optimal time of day for you to get your dose of sunshine, and the appropriate duration of exposure. The Circadian app also helps you identify peak UVB times in your location.
The standard public health advice is to avoid midday sun exposure, and to get sun exposure only in the early morning or late afternoon. But if we take into account the varying proportions of UVA and UVB radiation throughout the day, this advice is completely arse-about. (Shocker, I know.) UVB radiation is at its peak at midday, when the sun is at its highest point in the sky. Therefore, a short exposure to sunlight at this time of day will produce more vitamin D than longer exposures at other times of day. And that means less exposure not just to UVB but to UVA radiation, which penetrates into deeper layers of the skin than UVB, causing sunburn, premature aging and damage to the DNA of skin cells, and increasing the risk of skin cancer. Conversely, if you try to get your 'dose' of sunshine in the morning and afternoon, you'll be exposed to proportionately more UVA, which is more strongly implicated in malignant melanoma than UVB.
Facial skin not only shows the aging effects of sun exposure - wrinkling and pigmentation - much more graphically than skin on the body; its small surface area and lower 7-dehydrocholesterol content makes it less effective as a site of vitamin D production. So protect your facial skin by wearing a broad-brimmed hat whenever you're out in the sun.
On the other hand, skin that's not normally exposed to the sun will synthesise more cholecalciferol than regularly-exposed skin; a suntan results from increased production of melanin, the skin's natural UV-absorbing sunscreen. And when you lie down, more skin surface area is exposed to the sun's rays than when you're standing up or walking.
So the ultimate recipe for safe sunbathing to maximise cholecalciferol production and minimise the risk of melanoma, is to lie outdoors in a bathing suit, at the time of peak UVB, for just the duration of time required to produce the equivalent of 1000-5000 IU of oral vitamin D3. Then promptly cover up, seek shade or go inside, or, as a last resort, apply a mineral (i.e. not chemical) sunscreen2.
Eating your D
Cod liver oil
Cod liver oil was recognised in German medical literature as a dietary treatment for rickets as early as 1824, based on folkloric traditions (yes, doctors used to pay attention to remedies used by laypeople, rather than dismissing them as foolish superstitions). It is by far the richest dietary source of vitamin D in the form of cholecalciferol (vitamin D3). However, the concentration of cholecalciferol is highly variable depending on season, batch and manufacturing processes. Analysis of a cod liver oil supplement implicated in three cases of vitamin D intoxication, found that each capsule contained roughly one thousand times as much vitamin D as was declared on the label; the vitamin D content in capsules from other batches of the same product was as declared.
Furthermore, cod liver oil also contains vitamin A, and the level of vitamin A is similarly variable. According to the US Department of Agriculture's food database, 1 tablespoon of cod liver oil contains, on average, 1360 international units (IU) of vitamin D and 13600 IU of vitamin A, which exceeds the upper tolerable intake level (UL) of 10 000 IU for vitamin A. And that's no joke:
"Although the active metabolite of vitamin D requires binding to the retinoic acid receptor in order to function in gene transcription, high doses of vitamin A antagonize the action of vitamin D, probably at the site of the vitamin D receptor [127]. In humans, even vitamin A in a single serving of liver impairs vitamin D’s rapid intestinal calcium response [128]. In a recent dietary intake study, Oh et al. found high retinol intake ablated vitamin D’s otherwise protective effect on distal colorectal adenoma [129], and in that study they found a clear relationship between vitamin D and vitamin A intakes: the women in the highest quintile of vitamin D intake also ingested around 10 000 IU of retinol/day.
The consumption of preformed retinol, even in amounts consumed by many Americans in fortified low-fat dairy products, eggs, fortified breakfast cereals, multivitamins, and fish liver oil appears to be causing low-grade, but widespread, bone toxicity [130]. Further, a review of 67 randomized controlled trials involving 230 000 participants found vitamin A significantly increased total mortality [131], with antagonism to vitamin D a potential mechanism."
OK, so cod liver oil is not a good choice for obtaining vitamin D. What about whole foods?
Other food sources of vitamin D3
The fish species that contain relatively high amounts of cholecalciferol, such as farmed rainbow trout and sockeye salmon, are too expensive to be used as a primary dietary source of vitamin D (at $70 per kg for sockeye salmon which contains 563 IU of vitamin D3 per 100 g, you'd be shelling out $12.40 per day just to get 1000 IU). And then there's the problem of contamination of fish - especially the large, long-lived, predatory fish species that tend to have the highest vitamin D levels - with environmental toxins such as mercury, polychlorinated biphenyls, dioxins, microplastics, as well as antibiotics and other drugs. Fish oils can be purified to remove such contaminants, but fish itself cannot.
The other vitamin D
None of the other food sources of vitamin D3 contain sufficient concentrations of it to make a meaningful contribution to vitamin D nutriture, but there is one type of food that yields another calciferol compound - ergocalciferol, or vitamin D2 - that can be converted into 25-hydroxyvitamin D2 and thence into calcitriol: mushrooms. Strictly speaking, 'shrooms do produce cholecalciferol, as well as yet another related compound, 22-dihydroergocalciferol, or vitamin D4, but only in small amounts.
Just as our own 7-dehydrocholesterol is converted into cholecalciferol via UVB exposure, ergocalciferol is produced from its precursor compound, ergosterol, when sunlight or another source of UVB shines on 'shrooms.

The problem is, most commercial mushrooms are grown in the dark. Supermarket-bought white button mushrooms typically have less than 40 IU of ergocalciferol per 100 g fresh weight. However, wild-gathered mushrooms that receive some sunlight exposure can have much higher levels: 2348 IU per 100 g of porcini (Boletus edulis), up to 1200 IU per 100 g of funnel chanterelles (Cantharellus tubaeformis [Bulliard] Fries), and 428 IU per 100 g of golden chanterelles (Cantharellus cibarius [Fries]).
And you can juice your store-bought mushrooms up with ergocalciferol simply by putting them out in the sun during peak UVB periods: even winter midday sun in Sydney generated 400 IU of vitamin D2 per 100 g of small, whole button mushrooms, while sliced button mushrooms reached 1300 IU of vitamin D2 per 100 g after an hour of midday sun, in mid-summer in Germany.
UV lamps that emit UVB (such as those used in aquariums and grow lights for indoor plants) significantly boost ergocalciferol levels in post-harvest mushrooms, often reaching 1600 IU per gram of dried mushroom. The gills of shiitake mushrooms generate more ergocalciferol than the stems or caps, reaching up 912 IU per g of dried weight. But oyster mushrooms are the king of fungi when it comes to ergocalciferol, generating up to 5600 IU per g of dried weight when sliced and exposed to 60 min of UVB lamp radiation. Conversion of ergosterol to ergocalciferol occurs faster at higher temperatures, with 35°C the optimal temperature for both shiitake and oyster mushrooms.
From now on, my home-grown oyster mushrooms are going to receive a dose of midday sun after harvesting!
Vitamin D2 levels in fresh mushrooms fall rapidly with refrigeration, so if you're planning on dosing your mushrooms with UVB from the sun or a UVB lamp, make sure you either eat them within a few days, or air-dry or dehydrate them promptly.
The bioavailability of ergocalciferol in UV-exposed mushrooms has been found to be equivalent to supplements, with no significant differences in increase of total 25-hydroxyvitamin D levels observed between supplemental vitamin D3 and vitamin D2, and mushroom vitamin D2 groups.
The vitamin D2-D3 controversy
Ergocalciferol is converted into 25-hydroxyvitamin D2, while cholecalciferol is converted into 25-hydroxyvitamin D3. Bearing in mind the as-yet unanswered question of whether we should be using serum 25-hydroxyvitamin D levels as a “biomarker of effect”, discussed in Part 3, there is conflicting evidence as to whether cholecalciferol raises total 25-hydroxyvitamin D levels more effectively than ergocalciferol.
A systematic review and meta-analysis concluded that while bolus doses (i.e. larger, less frequent dosage regimes) of cholecalciferol boosted serum 25-hydroxyvitamin D concentrations more than bolus doses of ergocalciferol, the difference disappeared when considering daily dosing studies (possibly because 25-hydroxyvitamin D2 has a shorter half-life, at least in some populations). A subsequent systematic review and meta-analysis found that daily dosing of cholecalciferol was more effective than daily dosing of ergocalciferol in raising total serum 25-hydroxyvitamin D in people with a body mass index (BMI) under 25, but the difference in effectiveness disappeared in overweight people. There may also be sex differences, with females having a greater response to cholecalciferol than ergocalciferol, compared to men. And some of the tests used to quantify 25-hydroxyvitamin D may not measure the two metabolites equally, with 25-hydroxyvitamin D3 being overestimated, and 25-hydroxyvitamin D2 being underestimated.
Just to complicate matters further, 25-hydroxyvitamin D2 binds less strongly to vitamin D binding protein than 25-hydroxyvitamin D3, resulting in higher levels of free 25-hydroxyvitamin D (remember, only the free form can be converted into calcitriol, to exert its hormonal effects). In mice, this led to greater bone volume and bone density in the group that was only exposed to ergocalciferol from weaning onwards, compared to mice given only cholecalciferol.
The implications of this for human beings are anyone's guess, since all humans are exposed to some cholecalciferol throughout their lives. But it is known that there's no significant difference in biomarkers of vitamin D effects, including serum calcium, phosphorus, alkaline phosphatase, or parathyroid hormone levels, between people supplemented with vitamin D2 and D3, even when those given D3 have a faster and greater total increase in 25-hydroxyvitamin D levels.
Although both 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 are converted into calcitriol by the same alpha-hydroxylase enzyme, there is a slight difference in the chemical composition: 25-hydroxyvitamin D2 is converted into 1,25-dihydroxyvitamin D2 [1,25(OH)2D2] while 25-hydroxyvitamin D3 is converted into 1,25(OH)2D3. And there do appear to be differential effects of the two versions of calcitriol, with 1,25(OH)D3 not only influencing the expression of more than twice as many genes than 1,25(OH)D2, but influencing different genes:
"Only 13% of down-regulated differentially expressed genes were common between the two treatment groups while 28% and 59% were uniquely down-regulated by vitamins D2 and D3, respectively... Vitamin D3 (but not vitamin D2) enhances the expression of genes involved in the interferon alpha response, [which] is highly relevant to susceptibility to viral infection."
However, this study found contradictory effects of cholecalciferol supplementation in different ethnic groups: in south Asians, an increase in serum 25-hydroxyvitamin D3 concentration stimulated immune responses, other than the interferon pathways, while in white Europeans, several immune pathways were suppressed in those taking vitamin D3.
If you've made it this far, congratulations! You have a long attention span and a high tolerance for ambiguity and uncertainty, which are both essential attributes to have when exploring scientific literature. And if you're scratching your head, wondering 'So what in the bloody hell am I supposed to do????', my answer is that you can't go wrong by going out in the sun to get your cholecalciferol production, and getting a regular hit of ergocalciferol by eating delicious mushrooms that have been prized by every traditional culture for both culinary and medicinal purposes!
In the next post, I'll discuss what is currently known about optimising the production of calcitriol, and its interaction with the vitamin D receptor.
And finally, this post has taken me approximately 15 hours to research and write. The breadth, depth and complexity of the vitamin D research literature is truly mind-bending. I make all my posts freely available to all readers, because I believe we all deserve access to information that helps us to take greater control over our health. But I rely on my small core of paid subscribers to provide this service to those who genuinely can’t afford it.
For information on my private practice, please visit Empower Total Health. I am a Certified Lifestyle Medicine Practitioner, with an ND, GDCouns, BHSc(Hons) and Fellowship of the Australasian Society of Lifestyle Medicine.
To learn more about the effects of specific wavelengths of light on human, animal and plant health, I recommend John Ott's highly readable book, Health and Light.
I don't recommend sunscreen use on a regular basis as it disrupts the body’s innate mechanism for sun protection - melanin synthesis - and also tends to encourage people to spend more time in the sun than is appropriate for their skin type. Physical barriers to sun exposure, such as clothing, hats and shade, are better. However, if you cannot avoid prolonged sun exposure, an aluminium-free mineral sunscreen (i.e. one that uses a mineral, usually zinc, to reflect the sun's rays) will protect skin from sun damage if used in recommended amounts and reapplied frequently.




Is it both UV’s that cause the skin to tan? Or one or the other?
I’ve always been told that D2 is inferior to D3, but now I’m not so sure. I do like mushrooms 🍄🟫. I was in Costco the other day and saw a display at the end of the aisle(that’s why they put them there) for a D3&K2 supplement that was plant based. That caught my attention as I thought D3 was from animal sources. Looking at the label it said it was made from lichens. Puzzling as lichens aren’t animals(nor vegetables). As all supplements, natural or otherwise, are manufactured using some chemical process, I guess anything is possible. Any thoughts?