The placebo paradox
The placebo effect is one of the most fascinating yet least-discussed aspects of health care. Can we master the placebo effect to promote healing?
One of the least-discussed facts among medical and health practitioners of both an orthodox and alternative bent, is that the placebo effect accounts for a significant proportion of the apparent therapeutic effect of many treatment modalities.
Medical doctors will often dismiss their patients’ reports of benefitting from herbal medicine or supplements or acupuncture with the flippant retort, “That’s just the placebo effect!”
Yet many of the drugs that they routinely prescribe don’t perform much better - or any better at all - than placebo, when tested in randomised, placebo-controlled trials.

In fact, as one medical wit observed,
“[Placebo is the] most effective medication known to science, subjected to more clinical trials than any other medicament yet nearly always does better than anticipated. The range of susceptible conditions appears to be limitless.”
Placebos and the placebo effect: Easy to define; hard to quantify
A placebo - Latin for ‘I will please’ - is “an inactive, harmless substance given to patients to make them feel better by the power of suggestion”. Starch or sugar pills, and saline injections, are prototypical placebos. In the case of treatments that use processes rather than products, sham procedures (such as sham surgery - simulating surgery without actually performing it, or sham acupuncture - inserting acupuncture needles into sites that are not acupuncture points), are used as placebos. Perhaps the most concise description of a placebo is this one:
"It is the form of a treatment without its substance."
The placebo effect has been described as "the response to the healing situation", but this is somewhat of an oversimplification. It's actually easier to quantify the true treatment effect than the true placebo effect, because "the healing situation" involves more than just the administration of a treatment.
In a randomised, double-blind placebo-controlled trial, participants are randomly assigned (e.g. using a computer-generated code) to receive either the active treatment or placebo. Neither they, nor any of the experimenters, know whether they are taking the placebo or the active treatment. At the end of the trial, the code is broken and outcomes in both groups are compared. Any additional benefit received by the active treatment group over the placebo group (e.g. greater reduction in serum cholesterol level, blood pressure or score on a standardised depression scale) is attributed to the true treatment effect.
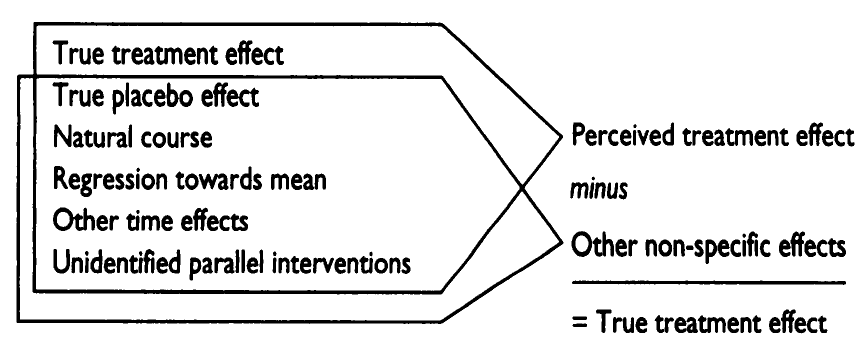
The remaining improvement in outcome - that is, the overlap between the treatment group and the placebo group - is often incorrectly attributed to the placebo effect. In reality, that overlap - the perceived placebo effect - is comprised of the true placebo effect plus several other non-specific factors including:
Fluctuations in the natural course of the disease - the innate tendency of conditions to either get better or get worse over time;
Regression towards the mean - the tendency of biological variables to move from extremes toward more normal values over time;
Other time effects such as seasonal variations in a biological variable or improvement in the skill of the investigator in measuring the variable; and
Unidentified parallel intervention - unconscious changes in behaviour made by participants, as a result of being enrolled in a clinical trial, that impact on the outcome.
Only after these effects are subtracted from the difference in outcome between the treatment and placebo groups, can the true treatment effect be determined:
It's worth noting that the perceived placebo effect may be of greater magnitude for participants in randomised clinical trials than in everyday clinical practice, because the nonspecific treatment effect of trial participation - which requires a recruitment process, information sessions, lots of form-signing and regular follow-ups - is likely much stronger than the commonplace experience of visiting a doctor.
Differentiation of the true placebo effect from the perceived placebo effect would require both a placebo group and a completely untreated control group. The untreated control group experiences all the nonspecific effects of participation in a clinical trial, without receiving a placebo or sham treatment. Hence, any additional benefits experienced by the placebo group over the untreated control group can be confidently attributed to the true placebo effect:
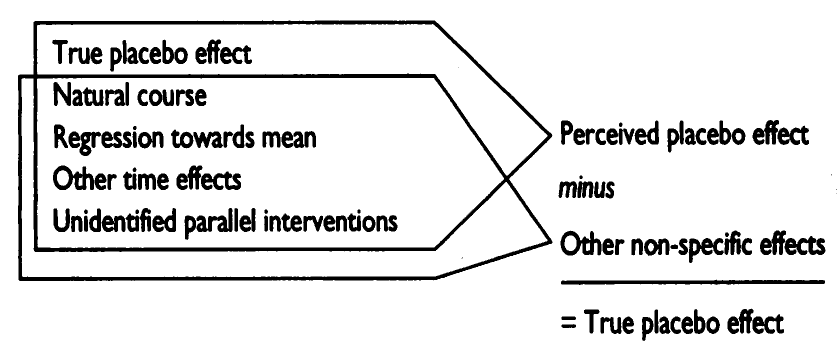
Unfortunately, a completely untreated control group is rarely included in randomised clinical trials, making it impossible to determine the magnitude of the true placebo effect in most studies.
Notwithstanding the conflation of nonspecific treatment effects with the true placebo effect, it's undeniably true that the placebo effect exists. That is, the administration of any form of treatment, whether that be a pill, an injection or a procedure, triggers some process that results in humans, at bare minimum, perceiving that they feel better than they did before undergoing the treatment.
Perhaps unsurprisingly, the aspect of illness that is most reliably responsive to the placebo effect is pain. Both oral placebos and sham procedures (for example detuned ultrasound equipment and sham acupuncture) have been shown to have substantial true placebo effects in terms of relieving pain.
In fact, in a triple-blinded, placebo-controlled randomised trial of adults with acute low back or neck pain, placebo was about as effective as opioid analgaesics after six weeks of treatment, and at 12-month follow-up, patients who had received an opioid analgaesic reported more pain than those who had been assigned to placebo.
And a systematic review and meta-analysis of randomised controlled trials of arthroscopic partial meniscectomy vs sham surgery (i.e. the surgical team pretends to perform the procedure while in reality only making a small incision in the knee) for degenerative meniscus tears, found that the surgery yielded only a small improvement over the sham group on knee pain at 24 months follow-up (2.5 points for the surgery group and 2.2 points for the sham group). There was no difference between the groups in overall knee function and health-related quality of life.
Moving away from pain, long-term readers might remember that, as I wrote in ‘Depressed’ or just going through a rough patch – have you been misdiagnosed?, "Irving Kirsch has argued convincingly in his book The Emperor’s New Drugs, careful study of clinical trials of antidepressant drugs indicates that they are no more effective than placebos." Hence it's also rather unsurprising that there's a strong response to placebo in many psychiatric diagnoses.
For example, a systematic review and meta-analysis published in May 2024 in JAMA Psychiatry analysed data from 90 high-quality randomised clinical trials, involving a total of 9985 participants with nine different psychiatric diagnoses. They found "significant improvement under placebo treatment for all 9 disorders", and that "the improvements were of considerable magnitude." Furthermore, the observed effect was "in a different order of magnitude than effect sizes resulting from the comparison of an intervention group with a control group, at least in psychiatry", indicating that the observed improvements in participants assigned to placebo were indeed true placebo effects, and conversely that the nonspecific factors discussed above were not significant contributors.
Patients with major depressive disorder had the most substantial response to placebo, with a Cohen's dav of 1.40. (According to Cohen’s criteria, a Cohen's d of 0.8 or greater is considered a large effect size.) Generalised anxiety disorder had the second greatest effect size (dav = 1.23), while participants with schizophrenia and obsessive compulsive disorder had the smallest response to placebo (dav = 0.59 and 0.65 respectively, which is still considered a medium effect size).
Importantly, despite the oft-repeated claim that "placebos do not generally have long-lasting effects and they do not cure diseases", the fact is that real physiological changes do take place in the bodies of people who take an inert substance or undergo a sham treatment that they believe has curative powers, and these physiological changes can result in significant alterations in the disease course.
For example, detuned ultrasound equipment was found to exert a significant true placebo effect on both swelling and C reactive protein concentration (a marker of inflammation) after tooth extractions. And both oral and topical placebos produced improvements in the objective signs of varicose veins, as well as the subjective symptoms, with topical placebo outperforming oral placebo.
Blood pressure, EEG parameters and serum hormone concentration have all been shown to be subject to placebo effects. Placebo-induced healing has been demonstrated, in randomised controlled trials, in conditions as diverse as angina pectoris, epilepsy and cancer - although once again, it's difficult to tease out the true placebo effect from the nonspecific factors described previously.
Astonishingly, even when patients are told that they are receiving a placebo - known as an open-label placebo - the placebo effect can still occur. Open-label placebos have been shown to induce the placebo effect (and therefore to elicit self-reported improvements) in chronic low back pain, knee pain, cancer-related fatigue, migraine headaches, irritable bowel syndrome and allergic rhinitis.
Powering up placebos
The most powerful true placebo effects are seen with:
Invasive procedures, such as sham acupuncture and sham surgery; injected placebos have a larger placebo effect than oral ones.
"Physical" placebos such as detuned ultrasound equipment.
Procedures that more actively involve the patient, such as self-applying a topical placebo cream.
These procedures are associated with more powerful true placebo effects than oral placebo administration.
Other influences on the extent of the true placebo effect include "the attitude of the doctor or therapist (towards the treatment and the patient),... the attitude of the patient (towards his or her own health, the doctor or therapist, the type of treatment),... the conditioning of the patient (his or her suggestibility), and... the type of treatment (its mechanism as well as impressiveness, invasiveness, perceived plausibility, experience, cost, etc)."
Having a higher proportion of female participants is also associated with larger improvements in placebo groups in clinical trials, suggesting that women may experience an enhanced placebo effect compared to men.
The diagnostic and prognostic capabilities of the practitioner also strongly influence the placebo response; the higher the confidence of the patient in the practitioner's accuracy in determining what's wrong with them and their likely response to treatment, the more powerful the placebo response.
These findings comport well with my clinical experience. Many of my clients have reported astonishing health improvements from treatments whose effectiveness I would consider dubious. Often, these results are gained after the practitioner uses a diagnostic device which, again, I would consider of dubious accuracy, but which the practitioner insists is incredibly accurate at quantifying all sorts of biological functions, and which impresses the client with its whiz-bangery. And my client population is roughly 90 per cent female. Hmmm.
All that said, the remarkable efficacy of placebo treatment in many health conditions should prompt the curious person to ask, "How does it work? And how might we make use of it?"
How the placebo effect works
Vital insights into the mechanisms of action of the placebo effect have been gained through research into antidepressant placebos. As mentioned previously, depression is exquisitely susceptible to the placebo effect.
In one fascinating study, participants with major depressive disorder, who were not taking antidepressant medication, were recruited into a trial in which they were informed that they would receive multiple brief infusions of a fast-acting antidepressant drug, while their mood response to the drug would be monitored using a visual neurofeedback device.
In reality, the infusion was simply saline, and the neurofeedback device was a sham. All participants received false 'feedback' which confirmed that the infusion was indeed improving their mood, either 25 percent of the time (low-reinforcement condition) or 75 percent of the time (high-reinforcement condition).
As researchers observed functional magnetic resonance imaging scans of participants' brains throughout the experiment, they were able to track the effects of positive expectancy (participants believed their mood would improve once the infusion commenced) and reinforcement (participants saw visual feedback that confirmed that their mood was improving) on blood flow signals in various regions of the brain.
In particular, a complex of brain centres called the salience network showed high activity throughout the experiment, correlating with self-reported improvement in mood. In a nutshell, the salience network was continually updating the expectancy of mood improvement as the experiment progressed, creating a positive feedback loop in which the more (fake) evidence was presented to participants that their mood was improving, the more they expected to experience further mood improvement, and the more their self-perceived mood actually improved:
"Our computational modeling revealed a positive feedback pattern where momentary improvements in mood, produced in part by sham neurofeedback evidence of an antidepressant’s rapid effects on the brain and in part by prior placebo expectancies, elevated people’s subsequent placebo expectancies."
Dynamic Feedback Between Antidepressant Placebo Expectancies and Mood
Similarly, in a series of trials of real vs sham neurostimulation via transcranial magnetic stimulation and transcranial direct current stimulation for depression and ADHD, participants' beliefs about whether they had received the active or sham treatment played a significant role in their outcomes. In fact, in some of the trials, participants' perceptions of receiving real or placebo treatment had more impact on outcomes than the treatments themselves.
Expectation of therapeutic benefit also plays a huge role in the response to pain medications and to psychedelic agents and MDMA too:
"It is difficult to separate expectations from true pharmacological effects for any treatment, and this is especially true for psychedelic drugs and MDMA, for which the profoundly subjective treatment effects cannot be blinded, and indeed likely underlie treatment effectiveness. Expectations can affect responses at every stage of psychedelic-assisted psychotherapy, and the drugs themselves may alter expectations and outcomes."
The Intricate Interaction Between Expectations and Therapeutic Outcomes of Psychedelic Agents
On a neurobiochemical level, our beliefs about the capacity of a particular treatment modality may be mediated via the endogenous opioid, neuroendocrine and psychoneuroimmune pathways. That is, optimistic thoughts and positive feelings about the treatment trigger the release of various neurochemicals which then switch on cascades of electrical and biochemical activity, resulting in conditions that facilitate healing and repair.
Recognising the power of positive expectancy to "switch on" our innate capacity for self-repair, we can think about...
How to maximise the placebo effect
May non-human animals spontaneously engage in zoopharmacognosy - intentionally self-medicating with plants and inorganic substances that do not form part of the usual diet, guided by some instinct that is beyond our ken. But since ancient times, humans have tended to seek out a "healer" of some description, rather than treating themselves. Hunter gatherers sought the guidance of shamans, pre-industrial peoples the intercession of priests, and most modern humans place their faith in doctors. Hence, one of the primary contributing factors to the placebo effect is the patient-practitioner relationship:
"The presence of a physician is the most common factor able to induce a placebo effect, the most frequently used ‘drug’ in general practice."
Placebos, Placebo Effect, and the Response to the Healing Situation: The Evolution of a Concept
Indeed,
"The administration of a placebo is neither a necessary nor a sufficient condition for the initiation of a placebo effect (3,146). Not only placebos but also any feature of the nonspecific elements (concomitants) of the physician–patient encounter may recruit the healing response. Hence, it is probably more appropriate to speak of the 'response to the healing situation' than of the 'placebo response'(3). Instead of, therefore, being conceptualized as the product of placebo administration (5), the placebo effect can be redefined as any effect attributable to the symbolic importance of a treatment, treatment setting, or treatment process (11). This reconceptualization bypasses the controversial issue of the existence or the magnitude of the placebo effect as it encompasses all the nonspecific influences."
Placebos, Placebo Effect, and the Response to the Healing Situation: The Evolution of a Concept
Conceptualising the "healing situation" in this way may resolve the thorny issue of differentiating the perceived placebo effect from the true placebo effect, since the entire process of seeking and receiving treatment is actually part and parcel of the induction of the placebo effect.
Hence, the relationship between you and any practitioner you consult is paramount. If your doctor, or any other medical or health practitioner, is cold, rude, arrogant, disrespectful, dismissive of your concerns, or a poor listener, you're very likely to obtain an inferior response from any treatment they prescribe or administer, than if they were warm, responsive, showed genuine interest in you, answered your questions thoughtfully, and demonstrated respect for your autonomy.
Beyond the practitioner-patient relationship, it's been my personal experience that people who immerse themselves in the study of the human body, and the factors which support its healing, have far better responses to treatment than those who are fearful of their body's normal and natural responses to dis-ease.
For example, once I learned about the profound healing effects of fever, I was never afraid of this symptom again, and never sought to suppress it with medication, either in myself or my children. Instead, I welcomed fever (despite its undeniable unpleasantness) as a powerful indicator of the body's vitality and capacity to fight off infection and restore homeostasis. In other words, my understanding of fever created a positive expectancy that the fever would soon be over after it had accomplished its purpose, and I, and my children, would be all the better for having experienced it. In every case, the "treatment" - bed rest, keeping warm during the initial phase of the fever response, abstaining from food, and at most a dab of lavender oil to relieve headache - was successful and, health was rapidly restored.
Likewise, people who take the time to research human nutrition thoroughly, taking into account our anatomy, physiology, biochemistry and evolutionary history, as well as epidemiological and clinical research, tend to experience much greater benefit from making dietary changes, than those who just glom onto the latest social media diet fad... and then the next one, and the one after that.
Learning about the specific benefits of changing your way of eating (or for that matter any other prerequisite for health, from physical activity to restorative sleep to spending time in nature) increases your positive expectancy that you'll receive those benefits once you make the change. You're more likely to notice incremental improvements in your well-being, which sets up a positive expectancy of further improvements, which then motivate you to continue with the new behaviour.
Ultimately, the placebo paradox boils down to this: placebos trigger a healing response to pain, psychological distress and illness, but that healing response is inherent. The program for self-healing is already written in every cell, just waiting to be activated by a) removing the causes of ill-health and b) providing the requirements for health, including the deep-seated trust that healing is possible.
Although, as mentioned before, a positive practitioner-patient relationship creates a more powerful placebo response, a good practitioner places the locus of control with the patient/client, empowering him or her to understand that it is through our own actions - not the intercession of some magic bullet - that we overcome disease and restore health.



Great article, Robyn! You are on point to identify that empowering our patients to understand their bodies helps the process of healing. We need more practitioners who care deeply and listen intently to their patients. Another excellent point that helps people to believe they can heal. Thank you for your time and dedication to keeping us all informed.
Great work, Robyn
Placebo: …”it is through our own actions - not the intercession of some magic bullet - that we overcome disease and restore health.”
And what of nocebo? I think everyone is familiar with that effect over the last four years. Media, government, big pharma, big medicine telling us that there was a deadly pathogen that came from bats and pangolins spreading and we were all going to die. Well, maybe not all of us. People became ill just because they thought they had been exposed.
People receive what they believe.
I think the power of our mind and body is more powerful than what most believe.