Pop quiz: Which of these two exposures is the bigger risk factor for a diagnosis of melanoma?
A: Getting too much sunlight on your skin
B: Having a high number of doctors who conduct skin checks in your area
Before you blurt out the answer, here's a clue:
Seek, and ye shall find.
Matthew 7:7
(I have always preferred the sonorous King James version of the Bible, with its 'ye's and 'thine's and 'verily's and 'begat's. It's just so much more... well, Biblical than the anaemic modern versions, which all sound like the Book of Cyril.)
Now, back to that pop quiz. If you picked option B, you've probably been reading my other articles about the rampant overdiagnosis of cancer, such as Major trial finds screening colonoscopy fails to ‘save lives’, Breast cancer screening – when ‘talking to your doctor’ may mislead rather than inform, New study on screening mammography shows more harms than benefits, PSA screening leads to unnecessary treatment… and suffering and Prostate cancer: duplicity, deception and betrayal.
And if you have read those articles, you won't be too surprised to learn of the findings of a nationwide analysis of melanoma incidence in the United States, published in JAMA Internal Medicine. Here's the punchline:
"In this cross-sectional ecological study of 727 US counties, melanoma incidence was weakly (or unexpectedly negatively) correlated with proxies for UV radiation exposure and was more strongly (and consistently positively) associated with proxies for diagnostic scrutiny. Counties with no dermatologists and shortages of primary care physicians had the lowest incidence, while counties amply supplied with both had the highest."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
Let's unpack this study together.
Firstly, it was coauthored by Dr H. Gilbert Welch, professor of medicine at the Dartmouth Institute for Health Policy and Clinical Practice, whose work I have cited extensively in my previous articles on cancer overdiagnosis. Dr Welch is a gadfly - although a humorous, affable and self-effacing one - to the medical-industrial complex, persistently nipping at the duplicitous and self-serving practices that increase its own wealth and power whilst eroding the health of the people who believe they are being served by it. I freely admit my own bias here, but in my opinion, anything that Dr Welch writes is worth reading.
Secondly, the study was a cross-sectional ecological analysis. This is a type of epidemiological (population-based) study that compares large groups of people, rather than individuals, at a single point in time, in order to identify relationships between a particular exposure - such as smoking, dietary pattern or use of a given drug - and a particular outcome - such as lung cancer, heart disease or birth defects. The 'groups' in this study were the 727 continental US counties that report to the Surveillance, Epidemiology, and End Results (SEER) Program (among a total of 3108 counties).
It's important to point out that because individuals don't actually participate in this type of research - that is, they aren't interviewed or examined in any way, unlike in other forms of epidemiological research such as cohort studies - the researchers have to figure out ways to approximate just how much exposure the population they're studying has had to the factors they're interested in. These are called proxy measures; more on that in a tick.
The other important thing to bear in mind is that this type of study design can only identify associations between exposures and outcomes. It cannot determine whether there is a causal relationship between the exposure and the outcomes. Hence, ecological studies are usually viewed as hypothesis-generating - that is, they identify an interesting association that other study designs can then explore in more detail, with the aim of determining whether a causal relationship actually exists.
In this study, there were two exposures of interest. The first was ultraviolet (UV) radiation exposure from that big fiery ball in the sky, upon which all life on Earth depends. The second was "diagnostic scrutiny", or how likely people were to have their skin checked by a doctor.
The researchers used three proxy measures for each of the two exposures.
For UV radiation exposure, they used
UV daily dose, a variable the National Cancer Institute specifically developed for melanoma analyses;
Cloud variability; and
Temperature variability.
For diagnostic scrutiny, they used
Median household income (an indicator of whether people can afford to seek medical care, in a country without universal health insurance);
Number of dermatologists per 100 000 residents of the county;
Number of primary care physicians (general practitioners) per 100 000 residents.
The outcome of interest was the incidence - that is, the occurrence of newly diagnosed cases - of melanoma in non-Hispanic Whites, the population group most susceptible to melanoma.
To sum up, Welch and his coauthors sought to find out whether the amount of UV radiation that the average white resident of a county was exposed to, and/or the likelihood of them seeing a doctor for a skin examination, was related to the incidence rate of melanoma in each county.
As expected,
"Proxies for UV radiation exposure changed gradually across geography."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
That is, the closer a county is to the equator, the hotter it gets in summer, and the less cloud cover it has, the more UV radiation exposure its inhabitants get. You're probably thinking, "Yeah, duh." But it was important for the researchers to verify that their proxy measures of UV radiation were accurate.
On the other hand,
"The UV daily dose, a variable the National Cancer Institute specifically developed for melanoma analyses, was uncorrelated with incidence."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
Hmmm. Interesting. So people living in counties which get more UV radiation exposure do not have a higher risk of developing melanoma; in fact, in some instances an inverse correlation was found - that is, melanoma incidence was lower in high UV-exposed counties. But wait, it gets even more interesting than that:
"Melanoma incidence and proxies for diagnostic scrutiny changed abruptly across contiguous counties."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
In other words, counties that were right next to each other had sharply different incidence rates of melanoma, even though their UV exposures were much the same. What could possibly be causing this disconnect between UV exposure and melanoma diagnoses? Let's read on:
"Counties with no dermatologists and shortages of primary care physicians had the lowest incidence, while counties amply supplied with both had the highest, despite having lower mean UV daily dose."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
Let that sink in. More doctors but less sunshine = higher incidence of melanoma diagnoses.
OK, but maybe if you live in a county with fewer skin doctors and GPs, you're less likely to be diagnosed with a melanoma at an early stage, when it's more treatable. In that case, we'd expect to see a higher rate of deaths from melanoma in such counties. But no,
"There was little association between melanoma incidence and melanoma mortality."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
Yikes. But maybe the researchers were working with incomplete data sets that weren't capable of yielding accurate information. Ah, but they thought of that. As a 'computer check', they examined whether smoking rates in each county were correlated with lung cancer incidence and death, and found that, indeed,
"Smoking prevalence was highly correlated with lung cancer incidence in the same counties... [and] the analogous association [i.e. between smoking rates and death from lung cancer] in lung cancer was strong."
Association of UV Radiation Exposure, Diagnostic Scrutiny, and Melanoma Incidence in US Counties
OK, not a data accuracy problem then. There really is only one conclusion to be drawn from the data: You're more likely to be diagnosed with melanoma if you live in an area with plenty of doctors, than if you live in an area with plenty of sunshine.
Once again, as with breast, prostate and bowel cancer, what we're apparently looking at here is an overdiagnosis problem: many people are being diagnosed with, and treated for, melanoma - the most feared form of skin cancer - when what they actually have is skin lesions that would never have gone on to cause serious illness or death if they had simply been left alone.
The consequences of overdiagnosing melanoma are not trivial:
Surgery can be disfiguring, costly in some locations, and carries unavoidable risks.
Topical treatments, oral and intravenous drugs used in melanoma treatment all have side effects that range from minor to life-threatening, and can also be expensive.
Just being told that you have a form of skin cancer that can be fatal is highly stress-inducing.
If you follow the strict sun avoidance advice issued by most skin cancer specialists after your (over)diagnosis, you'll have both reduced quality of life and biological consequences, such as reduced vitamin D and nitric oxide synthesis, which will put you at risk of a slew of other health problems.
And all of this for no reduction in the risk of dying of melanoma.
But is this study an anomaly? No, it's not. The fact is, there is scant evidence that either sun avoidance or visual skin examination by a clinician reduce the risk of dying of skin cancer.
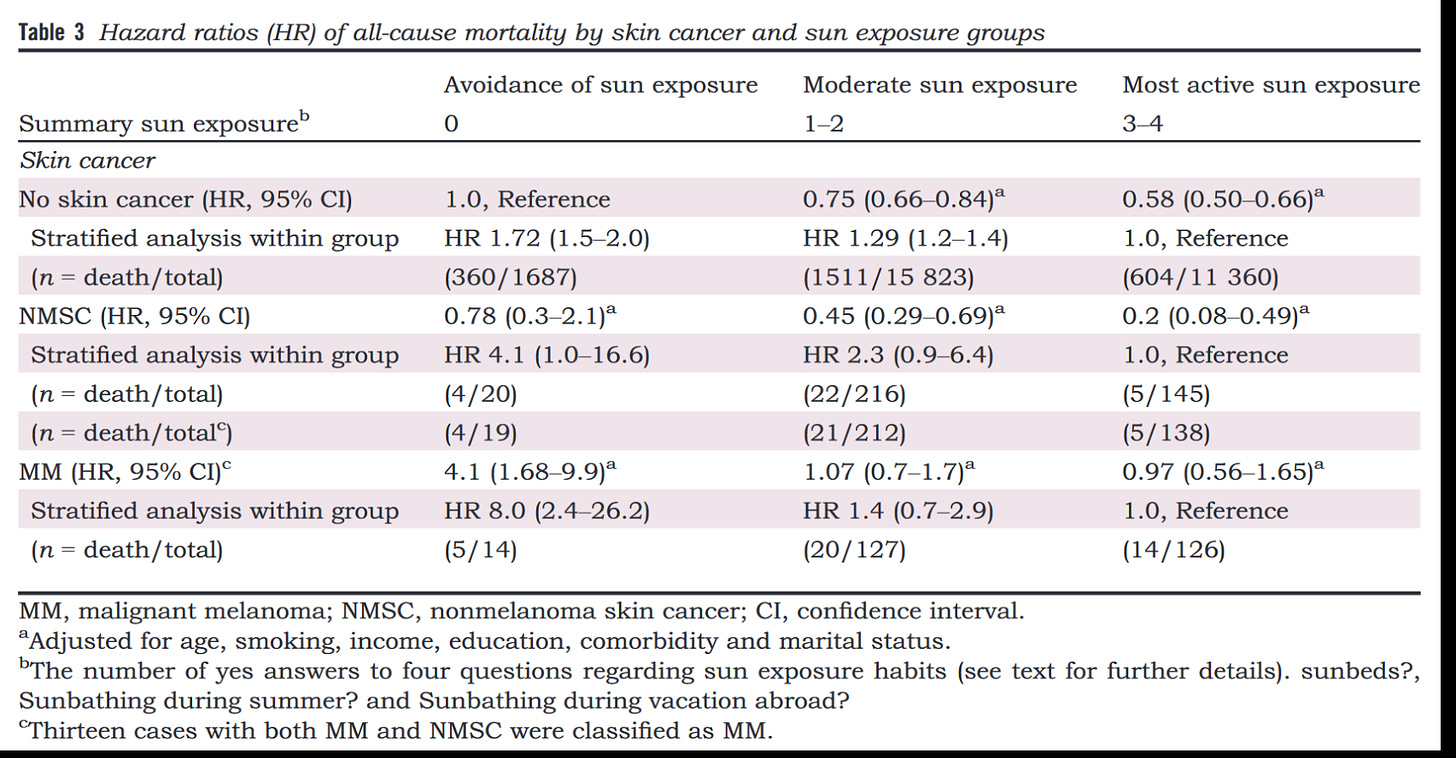
Furthermore, a prospective 20-year follow-up study of nearly 30 000 Swedish women, the Melanoma in Southern Sweden (MISS) cohort, found that
"Women with the most active sun exposure habits with NMSC [nonmelanoma skin cancer] were at the lowest probability of death, that is the group with the highest life expectancy. The HRs [hazard ratios] decreased dose dependently in both non-MM [non-malignant melanoma] and MM [malignant melanoma] groups with increasing sun exposure, with fourfold lower HRs amongst those with the most active sun exposure habits."
Check this out:
Notice that women who had nonmelanoma skin cancer but got the most sun exposure had an 80 per cent lower hazard ratio for dying of any cause, than women without skin cancer who avoided the sun. And that there was a trend to decreased risk of death in women with melanoma who got more sun exposure (although this didn't reach statistical significance; note how the confidence interval - the two numbers in parentheses - crosses zero in both the moderate and most active sun exposure groups).
Here's the real kicker:
"Nonsmokers who avoided sun exposure had a life expectancy similar to smokers in the highest sun exposure group, indicating that avoidance of sun exposure is a risk factor for death of a similar magnitude as smoking."
Again, let that sink in. Following 'doctor's orders' to stay out of the sun is as detrimental to your longevity as smoking.
(By the way, I discussed the many benefits of getting out in the sun in a webinar that I ran for my EmpowerEd membership group, called 'Let The Sunshine In: The surprising benefits of sunlight exposure'. You can watch this webinar, and hundreds of hours of other educational content on health and nutrition, by taking advantage of the 1-month free trial of EmpowerEd membership.)
So, now that we've established that the Welch et al study is not an anomaly, and that its findings comport with evidence gathered from a completely different study design, it's time to ask cui bono - who benefits from aggressive diagnostic scrutiny for skin cancer?
Many of the tentacles of the medical-industrial complex get to cash in: the doctors who conduct the skin checks, the pathology labs that analyse the biopsies, the surgeons who cut out the tumours, the oncologists who administer chemotherapy, and of course the pharmaceutical companies that make the treatments for skin cancer.
The public health apparatus benefits in a less obvious but perhaps equally important way: entire departments of (presumably) well-intentioned but woefully ignorant busybodies are kept in taxpayer-funded employ, to design social marketing campaigns that hector the public to stay out of the sun, and to subject themselves to frequent medical encounters for pointless skin checks1. And thus has the state managed to insert itself into yet another domain of our lives, arrogating to itself the right to weigh in on whether and how we should engage in one of the most enjoyable and beneficial (and free) activities known to humankind - getting out in the sun2.
Who doesn't benefit from aggressive diagnostic scrutiny? All the people dutifully attending for screening3. Big surprise there.
As a long-time advocate for evidence-based medicine that actually serves the interests of the patient (what a concept), Welch has some stern words for those participating in the skin cancer diagnosis industry. He and his coauthors call on melanoma researchers to “focus on the feared outcome of the disease” rather than just ginning up the number of cases through overdiagnosis, and urge clinicians and public health officials “not to exaggerate the magnitude of cancer risk factors, particularly for exposures as ubiquitous as the sun.”
Incidentally, one of those coauthors is Heather Welch, whom I presume is Gilbert's daughter. I for one am glad that there is a junior Welch gadfly to carry on her Dad's fine tradition of asking awkward questions and pointing out the nakedness of the emperor bestride the medical-industrial complex.
For information on my private practice, please visit Empower Total Health. I am a Certified Lifestyle Medicine Practitioner, with an ND, GDCouns, BHSc(Hons) and Fellowship of the Australasian Society of Lifestyle Medicine.
In Australia, we've been pummelled with ubiquitous Slip-Slop-Slap messaging since the 1980s; with typical bureaucratic mission-creep, the slogan has now expanded to Slip, Slop, Slap, Seek, Slide. I kid you not.
It goes without saying that your skin type determines how much sun exposure you can tolerate. If you’re a freckle-faced redhead, you’ll be burnt to a cinder long before your olive-skinned friend has just started to turn vaguely pink. And UV exposure does accelerate skin aging. If you don’t want to look like a wrinkled old prune before your time, wear a broad-brimmed hat to protect your facial skin, but let those arms, legs and torso soak up the rays, up to the tolerance level of your particular skin type.
As emphasised in my previous articles on overdiagnosis of cancer, screening is not the same as diagnosis. If you notice a skin lesion that is rapidly growing, changing colour, causing you pain or irritation, or behaving in any other fashion that causes you concern, get it checked by a competent doctor (preferably one who doesn't make a sizeable chunk of their income from diagnosing and treating such lesions).




As always, incredible article Robyn! It is so fascinating to see all these official "health recommendations" which actually do more harm than good.
"Take the vaccines!"
"The sun is dangerous, do not dare to spend too much time in the sun!"
"Visit doctors frequently to check for cancers, so if we find something, we can treat aggressively, thereby destroy your health and your immune system,, even if the finding would never have caused significant problems or may have reversed with time!"
"Ivermectin does not work and is dangerous!"
"Drink fluoridated water!"
etc. etc. etc.
The list is endless. All these recommendations do more harm than good. Is all that just a coincidence?
Sun exposure helps preventing many diseases and cancers.
"We observed a decreased risk of breast cancer for individuals spending ≥1h/d in the sun during summer months over a lifetime or usual adulthood compared with <1h/d [pooled relative risk (RR)=0.84; 95% CI: 0.77, 0.91]. Spending ≥2h/d in the sun had a similar protective effect as 1 to <2h/d when compared with <1h/d (RR=0.83; 95% CI: 0.75, 0.93 vs. 0.83; 95% CI: 0.78, 0.89). "
Hiller TWR, O'Sullivan DE, Brenner DR, Peters CE, King WD. Solar Ultraviolet Radiation and Breast Cancer Risk: A Systematic Review and Meta-Analysis. Environ Health Perspect. 2020 Jan;128(1):16002.
Spending time in the sun increases Vitamin D which reduces Melanoma risks.
"The prevalence of vitamin D deficiency was significantly higher in patients with melanoma than that in controls (odds ratio, 2.115; 95% CI, 1.151–3.885). In terms of prognosis, serum vitamin D levels were significantly higher in melanoma patients with lower Breslow thickness (≦1 vs. >1 mm: SMD, 0.243; 95% CI, 0.160–0.327). Moreover, melanoma patients with lower vitamin D levels had a significantly higher mortality rate (hazard ratio, 1.558; 95% CI, 1.258–1.931).
Vitamin D deficiency is associated with higher Breslow thickness and mortality in melanoma patients."
Tsai TY, Kuo CY, Huang YC. The association between serum vitamin D level and risk and prognosis of melanoma: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2020 Aug;34(8):1722-1729.
I also consider this new meta analysis interesting. Prophylactic supplementation of Nicotinamide/Niacinamide, a form of Vitamin B3, may reduce the risk of skin cancers, especially cutaneous squamous cell carcinoma and basal cell carcinomas. There was also a trend towards lower risk of melanoma, not reaching statistical significance, probably due to the low number of studies and events.
"Results: We screened 4730 citations and found 29 trials (3039 patients) meeting inclusion criteria. Nicotinamide was associated with a significant reduction in skin cancers compared to control (rate ratio 0.50 (95% CI, 0.29-0.85; I 2 = 64%; 552 patients; 5 trials); moderate strength of the evidence)."
Mainville L, Smilga AS, Fortin PR. Effect of Nicotinamide in Skin Cancer and Actinic Keratoses Chemoprophylaxis, and Adverse Effects Related to Nicotinamide: A Systematic Review and Meta-Analysis. J Cutan Med Surg. 2022 May-Jun;26(3):297-308.
Thanks for this fascinating take on the diagnostics. As someone who is pretty much outside of the the health care sphere (I have coverage but have not needed to go to a doc in many years), I self-diagnosed some unusual spots on my face and used petty spurge (Euphorbia sp.) topically. the spots reddened, blistered, scabbed, then eventually fell off, leaving no evidence of melanoma or 'weird' spots. I get outdoors daily, have also spent a life working outdoors. These days, I wear a hat and long sleeves for part of the day, but feel like I do get pretty consistent D3. I don't think it requires hours in the sun to get it. I wondered about those 'free skin checks' in Australia and wondered if I was missing out when visiting there for several months.