Major study finds that cancer screening programs don't extend life
A very large meta-analysis has found that people who get screened for cancer don't live any longer than those who don't.
If you scroll through my previous posts on cancer-related topics, you'll notice that many of those posts discuss the dismal outcomes of cancer screening programs.
For example, in A quick update on skin cancer screening and melanoma incidence and Skin cancer checks: life-saver or scam?, I discussed the lack of evidence that screening people for melanoma prevents deaths from that dreaded form of skin cancer.
And in Major trial finds screening colonoscopy fails to 'save lives', I shared the findings of a long-running trial which concluded that screening colonoscopy reduces the risk of being diagnosed with colorectal cancer, but not the risk of dying from it.
In New study on screening mammography shows more harms than benefits and Breast cancer screening – when ‘talking to your doctor’ may mislead rather than inform, I outlined the clear evidence that screening mammography does not reduce the risk of dying, either of breast cancer or anything else, of women who undergo it.
And in Prostate cancer: duplicity, deception and betrayal, I discussed the similar lack of benefit of prostate cancer screening for men.
For those of you who struggle to understand how cancer screening - which aims to find cancers when they are at an earlier stage, and therefore should be more easily treatable - could possibly be such an abject failure, I explained the reasons for this failure in quite some detail in Major trial finds screening colonoscopy fails to 'save lives'. I encourage you to read (or re-read) that article to familiarise yourself with the decades of evidence that cancer screening has manifestly failed to deliver on its promise of 'saving lives' (although it has certainly delivered big bickies for the medical technology companies that produce cancer screening equipment and tests, the medical practices that deliver those tests, and the politicians who buy votes by directing public funds to pointless and possibly counterproductive cancer screening programs).
In that article, I discussed a 2002 paper which examined 12 randomised controlled trials of cancer screening, and found that:
"In five of the 12 trials, differences in the two mortality rates [that is, cancer-specific mortality vs all-cause mortality] went in opposite directions, suggesting opposite effects of screening. In four of these five trials, disease-specific mortality was lower in the screened group than in the control group, whereas all-cause mortality was the same or higher. In two of the remaining seven trials, the mortality rate differences were in the same direction but their magnitudes were inconsistent; i.e., the difference in all-cause mortality exceeded the disease-specific mortality in the control group. Thus, results of seven of the 12 trials were inconsistent in their direction or magnitude."
All-Cause Mortality in Randomized Trials of Cancer Screening
In August 2023, JAMA Internal Medicine published a meta-analysis which updates that 2002 paper with more recent cancer screening trials. The authors included 18 long-term randomised clinical trials of screening programs for colorectal, prostate, breast, ovarian and lung cancer, involving a total of 2.1 million individuals. Median follow-up periods for the trials ranged from 10 to 15 years - plenty of time for differences in lifespan between screened and unscreened people to emerge.
The specific outcome that the authors wanted to calculate was how much longer people live if they undergo cancer screening.
And their conclusions are absolutely dismal:
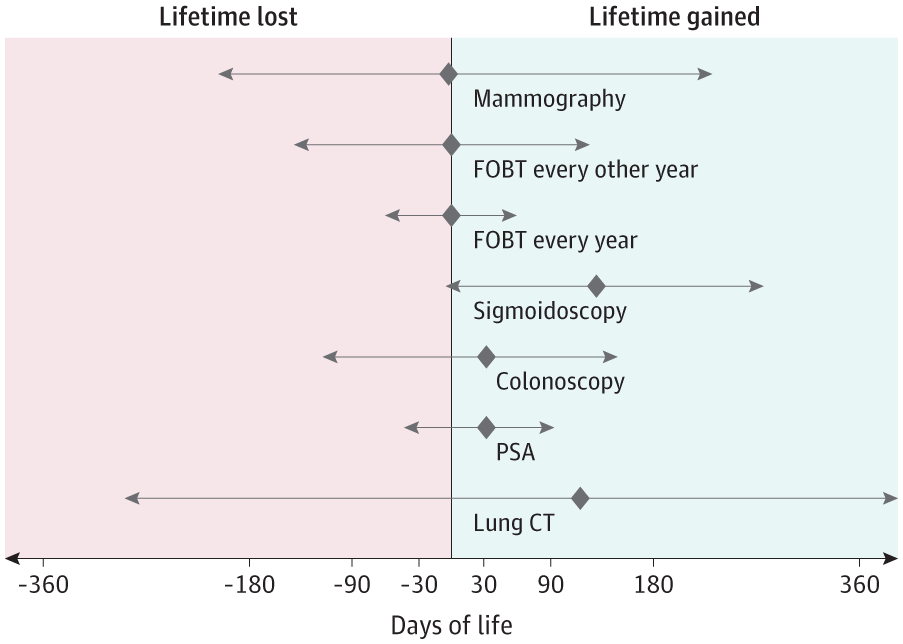
Only colorectal cancer screening using sigmoidoscopy delivered any life extension... but the gain in life expectancy was a meagre 110 days, or roughly three months.
Neither faecal occult blood testing (for colorectal cancer) nor mammography screening prolonged life.
There was a trend toward life extension for PSA testing (for prostate cancer) and colonoscopy screening (for colorectal cancer), but statistical significance was not reached because nearly as many screened individuals had their life expectancy shortened as had it increased. Moreover, the overall lifetime gain for screened individuals was a mere 37 days.
Likewise, lung cancer screening using computed tomography showed a trend toward increased lifespan - this time, a slightly more impressive 107 days - but statistical significance was again not reached, because so many screened individuals lived less long than unscreened individuals.
Figure 2 from the study tells the tale. The horizontal lines represent the range of outcomes experienced by participants, when data from all the studies was pooled for analysis. The diamonds represent the point estimate, or best guess of how much lifetime is gained or lost by undergoing that particular screening test. If the horizontal line crosses the vertical black line (the line of null effect), the results are not statistically significant - that is, it is possible that screening has no impact on life expectancy. Longer horizontal lines indicate fewer participants in the screening trial, and hence, lower confidence in the point estimate.
(If you'd like to learn how to decipher graphs like this, read this handy-dandy Tutorial: How to read a forest plot.)
The authors of the study are at pains to point out that some individuals experience a substantial increase in their lifespan by undergoing cancer screening. The problem is that a roughly equivalent number of people suffer a substantial decrease, either because the cancer screening test itself causes them harm (such as a perforated bowel from colonoscopy), or the treatment for the cancer that the screening test diagnosed, results in life-shortening damage.
Another reason why cancer screening fails to 'save lives' relates to the fact that screening tests do absolutely nothing to address underlying diet and lifestyle risk factors. Remember, screening is not prevention; it is (purportedly) early detection. And people who get the all-clear on their cancer screening test may be less likely to engage in health-promoting behaviours subsequently (the 'self-licensing' effect that I discussed in Major trial finds screening colonoscopy fails to ‘save lives’).
The risk factors for the most common types of cancer - obesity, sedentariness, smoking, alcohol consumption, insulin resistance - are also risk factors for cardiometabolic disease, which is a far greater cause of death than any individual cancer. An obese diabetic whose early-stage colorectal cancer is detected and successfully treated because of screening colonoscopy, may end up dying of a heart attack at roughly the same time as he would otherwise have died of cancer. The fact that this person did not die of bowel cancer would be touted as a victory by the advocates of screening, but that's cold comfort for him - dead is dead!
The authors call for greater transparency from policy-makers and healthcare providers when discussing the risks and benefits of cancer screening programs with the public. Currently, cancer screening is aggressively marketed to the public with false and misleading claims that these programs 'save lives'.
A shared decision-making process, in which individuals make decisions on which screening tests they will undergo, based on their own values, is the only ethical option. This is the approach that I have taken with clients since I began clinical practice in 1995. I explain the currently-known risks and benefits of any diagnostic tests, procedures and medications that have been recommended to each individual, as well as the tests and treatments that I recommend, and then leave each individual to make his or her own decision.
Sometimes my clients make decisions that I personally would not make, and sometimes I consider their decisions to be unwise. (For example, many of my clients allowed themselves to be injected with one or more COVID transfection agents, after I had discussed the known and suspected harms with them. Some are now paying a very high price for that decision.) But my opinion is irrelevant; every person has their own unique decision-making calculus, and it's not my job to try to alter the values on which this calculus is based.
Given the economic and political influences at play, it is highly unlikely that governments and insurers will stop wasting money and resources on cancer screening programs any time soon. If you want to reduce your risk of cancer (and other life-shortening diseases), it's up to you to take responsibility for your diet and lifestyle choices.
Eating more healthy plant foods such as vegetables and whole grains, minimising red and processed meat consumption, avoiding refined grains and added sugars, exercising regularly, maintaining a healthy weight, drinking little to no alcohol, avoiding smoking, and eschewing hormone replacement therapy have been found to reduce the risk of common cancers by 30 to 40 per cent.
And even more cancers could be prevented if all women breastfed their babies and then weaned them onto an optimal diet, and were (somehow) able to ensure that they followed this optimal diet for the rest of their lives, while also avoiding smoking and alcohol consumption, and engaging in regular physical activity. OK, good luck with all that.
But anyone, at any time, can choose to adopt habits which reduce their risk of developing cancer, or even arrest its growth if they already have it. What are you doing, and what do you plan to start or stop doing, to protect yourself against cancer? Let me know in the comments section below!




Another wonderful post! Not enough people are making these posts. The medicos just push more and more cancer screenings, tests, surgeries, chemo; you name it. And for what? At best, a measly few months of extra life, but that's just for the sigmoidoscopy (but almost ALL the patients have colonoscopies, anyway!), otherwise it effectively doesn't make a damned bit of difference. And who wants to spend a tonne of time in hospitals getting poisoned with chemo and seeing miserable 'doctors'?!
So I say get on with life, enjoy yourself, stress less - and of course do those healthy lifestyle things!
OK, so we don't eat a purely plant-based diet (we DO eat meat, but also plenty of organic plant food and we are dairy-free & soy-free & try to have no GMO foods + I make a lot of food from scratch), but we exercise, there's zero alcohol or smoking going on, I breastfed all my kids, they're adamant about eating well and having NO injections - ever - and they love sport! So perhaps in my family, even though my Mum has had countless skin cancers cut out/burned off, and my Dad had his prostate out in his 50s due to super high PSA, we tend to do the 'lifestyle' thing differently and thus may get different outcomes. I live in hope :-)
Why do many GP's have their "practice" next to a pharmacy? Personal responsibility for many people is a bridge too far; E.g jab uptake, trust in the government, that is all.