Previously in this series, I’ve discussed the origins of the ketogenic diet and the biological role of ketone bodies (Part 1), whether living in a state of ketosis is normal and natural (Part 2), whether ketogenic diets are effective for weight loss (Part 3) and insulin resistance and diabetes (Part 4), and whether ketogenic diets can cure cancer (Part 5). Now, let’s examine the impact of the high fat, low carbohydrate diet-style on the gut microbiome, and the health implications of long-term ketogenic diets.
First, a short primer on the human gut and microbiome. The term ‘gut’ means the entire gastrointestinal tract, from mouth to anus, but when we speak of ‘the gut microbiome’, we’re primarily talking about the microorganisms that inhabit our large intestine, or colon, and their genetic material. The stomach harbours very few bacteria under normal circumstances, due to its intense acidity, and the upper small intestine is also hostile to bacteria due to high concentrations of bile and other digestive juices.
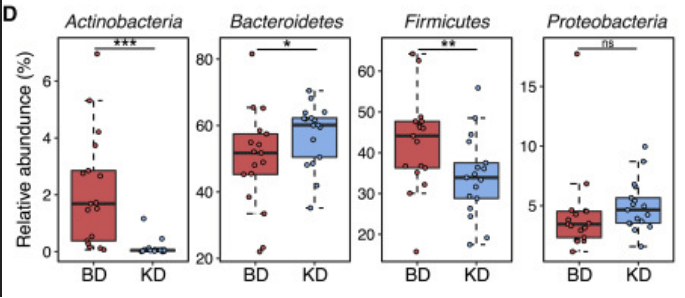
The large intestine, however, is a different story. It provides an ideal environment for bacteria: warm, moist, and full of food. There are over 1000 bacterial species in the human gut (in some people, up to 100 000 000 species), falling into 6 main ‘families’: Firmicutes (averaging 64% of gut microbiota), Bacteroidetes (23%), Proteobacteria (8%), Actinomycetes (3%), Verrucomicrobia and Archaebacteria (2% combined).
While there is no consensus on the ‘ideal’ composition of the human gut microbiome, there are particular patterns of imbalanced gut microbiota, known as dysbiosis – underrepresentation of certain bacterial species, and overrepresentation of others – which are strongly linked with a heightened risk of various diseases. Inflammatory bowel disease, obesity, type 2 diabetes, cardiovascular disease, and cancer are just some of the diseases that have been linked to imbalanced gut microbiota.
The overall diversity and specific composition of our gut microbiota are affected by numerous dietary components, including total protein and proportions of protein from animal vs plant sources; total fat and proportion of saturated vs unsaturated fat; fibre; resistant starch; polyphenols; and sugar.
The ketogenic diet is characterised by being high in fat, very low in carbohydrate, and very low to moderately high in protein (depending on whether it is a classical or modified ketogenic diet – see Part 1).
Fat
A high-fat diet has been found to reduce colon bacteria overall, while increasing total anaerobic microflora and Bacteroides counts. Bacteroides are normally beneficial organisms, but overgrowth is associated with inflammatory bowel disease, severe, antibiotic-resistant infections, and colorectal cancer.
A small study of people suffering from Glucose Transporter 1 Deficiency Syndrome (GLUT1 DS – a cause of epileptic seizures) found that after three months on a ketogenic diet, there was a significant increase in Desulfovibrio spp., a group of bacteria known to produce hydrogen sulphide – a gas which causes gut inflammation and is linked to the development of inflammatory bowel disease.
In a study of people at high risk of metabolic syndrome, switching from a diet high in saturated fat (typical of the ketogenic diet) to a low fat diet increased the numbers of beneficial Bifidobacteria, and this correlated with reduced fasting glucose and total cholesterol – in other words, a reversal of metabolic syndrome.
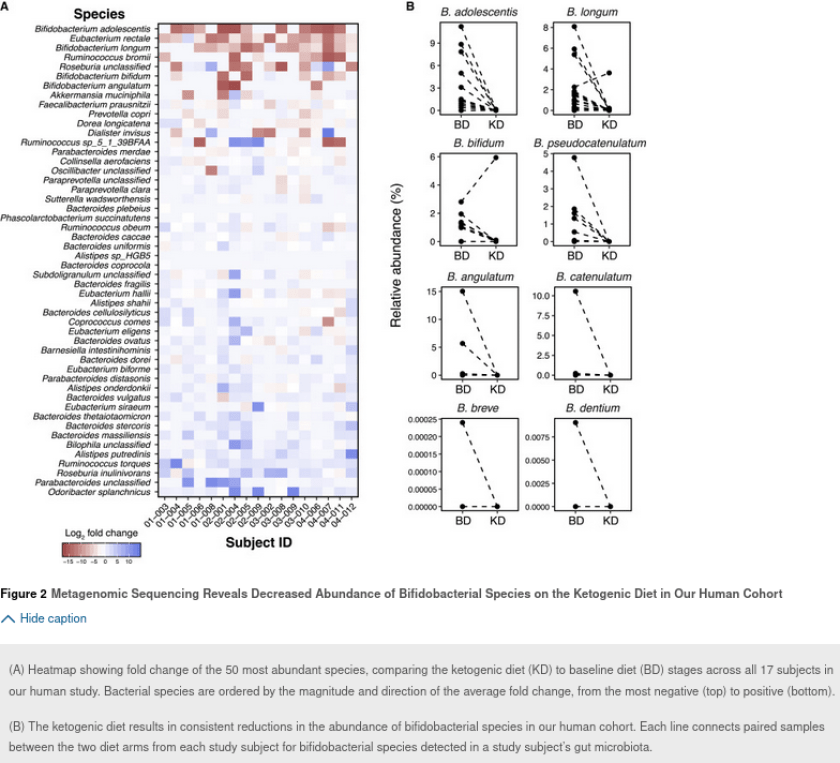
A ketogenic diet was found to significantly raise the abundance of Fusobacteria and Escherichia, which have both been implicated in predisposition to colorectal cancer, in the stool of human volunteers. At the same time, the ketogenic diet dramatically reduced the relative abundance of Actinobacteria, with those beneficial Bifidobacteria once again showing the sharpest decline:
A high fat diet increases intestinal permeability – that is, it causes leaky gut, by turning off the genes that code for proteins that comprise tight junctions, the ‘seals’ between neighbouring intestinal cells. Tight junctions are intended to stop unwanted or dangerous gut contents – such as undigested proteins and bacterial toxins – from leaking through the gut wall and into the bloodstream.
One of those bacterial toxins is endotoxin, a component of the cell walls of gram negative bacteria (including Bacteroides, Alistipes, and Bilophila). Saturated fat intake, in particular, increases the absorption of endotoxin from the gut into the bloodstream. The presence of endotoxin in the blood (endotoxaemia) is a powerful trigger of inflammation, and is associated with reduced glucose tolerance (which can eventually lead to diabetes), body weight gain, fat mass development and oxidative stress.
People suffering from major depressive disorder have been found to have higher levels of serum antibodies against endotoxin than non-depressed people, indicating leaky gut and an immune response to endotoxaemia.
Mice fed a high fat diet were found to become more vulnerable to anxiety-like behaviour. Although research linking high fat intake to anxiety in humans is lacking at present, the fact that mice suffer the same loss of microbial diversity on a high fat diet as humans do, and that this loss of diversity is correlated with anxiety in mice, should give serious pause for thought – especially given the simultaneous popularity of ketogenic diets and the explosion in the incidence of anxiety.
High fat intake also increases the amount of bile secreted by the gall bladder into the small intestine. This increases the relative abundance of bacterial species that use bile as a food source, including Bacteroides, Alistipes, and Bilophila. High counts of these bacteria are associated with increased inflammation. High counts of Bilophila wadsworthia has been linked to increased incidence and severity of colitis and colorectal cancer, while Alistipes was found to be overrepresented in people suffering from major depressive disorder.
On the other side of the scale, the therapeutic effect of ketogenic diets on drug-resistant epilepsy is believed to be largely attributable to their impact on gut microbiota. Likewise, some of the beneficial effects on markers and symptoms of neurodegenerative disease that have been observed in trials of ketogenic diets correlate with alterations in the composition of gut microbiota. Parents of children with intractable epilepsy may rationally decide that the imminent risk of brain damage from unrelenting seizures outweighs the long-term danger posed by adverse changes to gut microbiota.
But for everyone who is not thus caught between Scylla and Charybdis, serious consideration needs to be given to the known and unknown risks of long-term depletion of health-promoting gut microbiota that results from following a ketogenic diet.
Carbohydrate
Proponents of ketogenic diets tend to lump all carbohydrate-containing foods together, demonising them as the root cause of every chronic disease that plagues Westernised countries.
However, when it comes to the gut microbiome, all carbohydrates are not created equal. Unrefined or minimally-processed carbohydrate-rich foods, such as whole grains, starchy vegetables, legumes and fruits, contain non-digestible carbohydrates including fibre, resistant starch and non-starch polysaccharides – dubbed ‘microbiota accessible carbohydrates’ or MACs by pioneering gut microbiome researchers, Erica and Justin Sonnenburg.
Unlike simple starches and sugars, these non-digestible carbohydrates are not broken down by human digestive enzymes in the small intestine, and don’t serve as a food source for us. Instead, they make it all the way down to the large intestine where our gut microbiota ferment them, producing not only an energy source for themselves, but a plethora of compounds which are beneficial for their hosts – us.
A diet low in MACs reduces total bacterial abundance – one of the major indicators of a healthy gut microbiome – and microbiota gene richness. As Erica and Justin Sonnenburg put it, eating a low carbohydrate diet equates to “starving our microbial self”.
The consequences of this impoverishment in total numbers and diversity of gut bacteria are not yet understood, but it’s worth noting that humans who live a more ‘primitive’ hunter gatherer lifestyle, such as the Hadza of northern Tanzania, have far greater microbial richness and biodiversity than typical Westerners – a characteristic linked to their high consumption of fibrous plant foods, and strongly correlated with their freedom from typical Western diseases including obesity, diabetes and colorectal cancer.
One of the products of bacterial fermentation of MACs – specifically resistant starches and dietary fibre – is butyrate. Butyrate has an astonishingly diverse suite of benefits, including:
Providing the major fuel source to colonocytes (the cells lining the large intestine)
Maintaining the integrity of the gut lining (preventing and healing leaky gut)
Reducing mucosal inflammation
Reducing visceral hypersensitivity (the gut-brain communication disorder that underlies irritable bowel syndrome)
Modulating intestinal motility
Preventing and inhibiting colorectal cancer
Reducing serum cholesterol
Reducing insulin resistance
Assisting with weight loss
Preventing stroke
Increasing brain derived neurotrophic factor (BDNF), which stimulates the growth of new nerve cells and connections between existing ones.
Even ketogenic diets that are high in fibre-rich but low-carbohydrate vegetables cannot hope to achieve the quantity and diversity of MACs needed to cultivate a healthy and diverse gut microbiome. Non-fibre MACs such as resistant starch and non-starch polysaccharides are found most abundantly in whole grains, legumes and fruits, not vegetables.
The American Gut Project – a massive citizen science project which is using ‘big data’ to help fill in the gaps in our knowledge about the complex web of linkages between our diet and lifestyle habits, gut microbiota, and health status – reported in 2018 that the single greatest predictor of microbial diversity is the number of different plant foods eaten per week.
Participants who reported eating more than 30 different plant foods per week had the most diverse microbiota. It’s easy to eat this many different plant foods on a wholefood, plant-based diet, but virtually impossible on a ketogenic diet that excludes most fruits, starchy vegetables, whole grains and legumes.
Contrary to the constant refrain of low-carbers, whole grain consumption is consistently linked with improved health – including reduced risk of type 2 diabetes, cardiovascular disease, weight gain and colorectal cancer – and it is likely that many of the benefits of whole grain consumption are mediated through their effects on gut microbes.
For example, diets rich in whole grain and wheat bran are linked to an increase in the beneficial bacteria Bifidobacteria and Lactobacilli, while whole grain barley and resistant starch increase the abundance of butyrate-producing Ruminococcus, Eubacterium rectale, and Roseburia. And conversely, people who ate a high protein/low carbohydrate diet were found to have reduced Roseburia and Eubacterium rectale in their gut microbiota, and decreased butyrate in their faeces. Faecalibacterium prausnitzii, one of the key producers of butyrate, also thrives in the colons of people who eat diets high in microbiota-accessible carbohydrates.
The real-world effects of these diet-induced alterations in gut microbiota are serious and multifaceted. Here are just two examples:
People with advanced colorectal cancer were found to have lower counts of fibre-loving Roseburia and Eubacterium than cancer-free controls, associated with a lower fibre intake, and reduced levels of butyrate and other short chain fatty acids.
In a study comparing the gut microbiota of people suffering from major depressive disorder (MDD) to non-depressed people, depressed individuals had significantly fewer Faecalibacterium prausnitzii, Roseburia hominis and Roseburia intestinalis in their stool. Depleted levels of F. prausnitzii, in particular, were found to correlate with reduced capacity to produce butyrate, the ‘sleep hormone’ melatonin, and the neurotransmitters glutamate and gamma-aminobutyric acid, in people suffering from major depression.
A gluten free diet was found to decrease numbers of beneficial Bifidobacterium and Lactobacillus and increase counts of the opportunistic pathogens E. coli and Enterobacteriaceae, in healthy (non-coeliac) volunteers, after just one month. Clearly, people diagnosed with coeliac disease need to strictly avoid gluten in order to reverse the damage that has been done to their gut by the autoimmune reaction to this protein. However, non-coeliacs who have adopted a gluten-free diet because they wrongly perceive that it is ‘healthier’ may be doing themselves much more harm than good.
Protein
While the classic ketogenic diet is low in protein, some variants are relatively heavy on protein – almost invariably animal proteins, since plant proteins come ‘packaged’ with carbohydrate.
Bile-tolerant anaerobes such as Bacteroides, Alistipes, and Bilophila increase with consumption of animal-based protein, while the beneficial bacteria Roseburia and Eubacterium rectale are depleted by high protein, low carbohydrate diets – and consequently, lower butyrate production is observed in people following such diets.
Fewer butyrate-producing bacteria are found in the faeces of inflammatory bowel disease patients than healthy control patients. High animal protein intake has been found to significantly increase the risk of developing inflammatory bowel disease.
The dysbiotic pattern of increased Bacteroides and diminished butyrate-producing bacteria has also been identified in colorectal cancer patients.
Summary
High fat, low carbohydrate ketogenic diets cause major disruptions to the human gut microbiome, triggering leaky gut and systemic inflammation. Since the study of the gut microbiome is still in its infancy, the long term consequence of the dysbiosis induced by ketogenic diets are unknown, but strong links are already evident with a number of chronic diseases including inflammatory bowel disease and colorectal cancer.
Our ‘microbial self’ thrives on a diverse array of carbohydrates – fibre, resistant starch and non-starch polysaccharides – found only in plants. If you want a healthy gut microbiome, and all the benefits that flow from it, the solution is simple: Eat More Plants.




Perhaps the last sentence could read, ‘Eat more plants that are free from glyphosate, atrazine and paraquat.’
How does one find out what their gut composition is ? Pathology test ? Or are there home test kits ?
“where our gut microbiota ferment them” - is flatulence a sign of a healthy or unhealthy gut or “depends” ? I seem to recall that the Kalahari bushmen in the Gods Must be Crazy were avid “farters” but I dunno if that was done for exaggeration