Diving down the low-carb rabbit hole - Part 2
I continue my analysis of Dr Paul Mason's presentation on "seed oils" and heart disease.
Let's pick up where I left off in Part 1 of this mini-series dissecting claims made by Dr Paul Mason in his presentation, Decoding Atherosclerosis: The clotting theory and seed oil toxicity.
13:30: "The size and density of LDL however changes when it becomes damaged, of which oxidation is a major cause. In this sample, you can see four distinct populations of LDL, exactly three more than normal, representing the presence of oxidised and therefore damaging LDL particles. This LDL is often referred to as small, dense, given they become microscopically smaller."
Mason argues that oxidation causes "normal", supposedly harmless, LDL to become dangerous, atherogenic small, dense LDL. But in fact, the relationship between them is exactly opposite to his formulation:
"Low-density lipoproteins (LDLs) are susceptible to structural modifications by oxidation, particularly the small dense LDL particles."
In other words, it's the small, dense LDL that promotes oxidation, not the other way around.
And furthermore, having a higher blood level of linoleic acid, the omega-6 fatty acid found in abundance in those dreaded "seed oils" is associated with having lower small, dense LDL:
"Total n−6 PUFAs [omega-6 polyunsaturated fatty acids] and LA [linoleic acid] were significantly and inversely associated with total and small LDL particle concentrations and significantly and positively associated with large LDL particle concentration and LDL size."
Or, in English, the higher the level of fatty acids associated with "seed oil" intake, the lower the level of the dangerous small, dense LDL particles and the higher the level of the benign large and fluffy LDL.
In a randomised controlled trial of people with elevated levels of small, dense LDL particles (a high-risk profile for atherosclerotic cardiovascular disease, described as "LDL phenotype B"), a moderate carbohydrate (39 per cent of daily calories), very high saturated fat diet (36 per cent) diet further raised blood levels of small, dense LDL after three weeks. Conversely, a low saturated fat diet (37 per cent carbohydrate, 9 per cent saturated fat) reduced small, dense LDL particle number. Plasma concentrations of the atherogenic particle, apolipoprotein B, rose by 9.5 per cent in the high saturated fat group, and dropped 6.8 per cent in the low saturated fat group.
Well, that doesn't fit Mason's narrative, does it?
13:58: "While most people people who have heart attacks have normal total levels of LDL, there being no difference in LDL levels with or without a heart attack, when we look at damaged or oxidised LDL it's a different story. Look at the level of damaged LDL in the group on the left who don't have heart disease. Compare it to the oxidised LDL level in the two groups on the right who do have heart disease. Chalk and cheese."
I've already discussed Mason's deceptive use of the term "normal" in relation to LDL-cholesterol (see discussion of 1:44 in Part 1), so I won't rehash this argument.
This is the study from which Mason took the diagram he showed in his presentation, and here is the diagram:
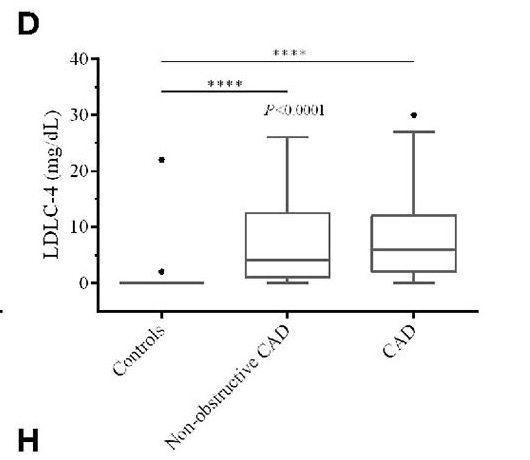
You'll notice that there is no mention of "oxidised cholesterol" on that diagram. The biomarker that was measured was LDLC-4, a subfraction of LDL-cholesterol that is classified as small, dense LDL, which, as you'll remember from the previous point, is not a product of oxidation, but a molecule that is particularly susceptible to it.
And in fact, you won't find the terms "oxidised", "oxidized", "oxidation" or "oxidative stress" anywhere in this article. Go ahead and search it for yourself. The only instances of "oxi" you'll find are in the references section. Mason has completely misrepresented this study in order to bolster his argument that people should be focusing on oxidation products rather than their LDL-cholesterol level.
14:27: "An oxidised LDL or of course any other blood oxidation product is also able to damage this furry layer that lines blood vessels, called the glycocalyx... The fact that oxidised LDL damages the glycocalyx means it significantly increases the risk of clotting and therefore atherosclerosis."
Once again, Mason fails to mention that oxidised dietary cholesterol - that is, cholesterol that was already oxidised at the time it was consumed, in the form of cooked animal products - is a more persistent blood oxidation product than oxidised fats (discussed above, in the discussion notes for 9:47). Why doesn't he mention this? Because it doesn't suit his argument that “seed oils”, rather than constituents of animal-derived foods, drive atherosclerosis.
It's also important to note that inflammation, rather than oxidative stress, is thought to be the initiating event in glycocalyx damage, with oxidative stress occurring as a consequence of inflammation.
15:13: "Oxidation stress too appears to be the cause of calcification within arteries. Oxidation has been shown to lead to DNA damage which leads to the expression of a chemical moiety called poly(ADP-ribose), and this then lays down calcium within the lining of the arteries. That coronary artery calcification is associated with unstable plaques and heart attack is therefore probably not a coincidence."
This is a gross oversimplification of a complex topic. Whilst it is certainly true that spotty calcification, which occurs early in the development of atherosclerosis, is associated with plaque instability and increased risk of heart attack, more extensive calcification is associated with stable plaques:
"Although there is overwhelming evidence that higher calcium scores are associated with a greater cardiovascular risk, at an individual plaque level, studies have shown that calcified plaques are more stable and less prone to rupture."
Detecting unstable plaques in humans using cardiac CT: Can it guide treatments?
In other words, a high coronary artery calcium score indicates extensive atherosclerosis, but it's not the heavily calcified plaques that are the riskiest: it's those with less, and more diffuse, calcification.
15:45: "Interestingly, statins are also known to damage DNA, a fact which was apparent to the Japanese scientists who stopped researching the mycotoxin that eventually became the first statin, because of the increased rate of cancer in test dogs. Which makes it unsurprising that statins also significantly increase coronary artery calcification."
While it is true that some of the dogs treated with mevastatin, the first statin, developed intestinal tumours, and that this halted trials of the drug, the reason for this was never discovered. Surprisingly, people with dyslipidaemia (unfavourable, pro-atherogenic cholesterol profile) actually show reduced chromosomal DNA damage after taking statins. Atorvastatin upregulates the activity of certain genes involved in the repair of damaged DNA.
In any case, Mason's attempt to link purported statin-induced DNA damage with increased coronary artery calcification is a complete non sequitur. He doesn't even attempt to explain how these two phenomena might be linked.
Mason cites this study which does, indeed, find that statins increase coronary artery calcification... in mice. There's now evidence that statin use increases the coronary artery calcium score (CACS) in humans too, with longer use associated with a higher CACS.
However, the study that Mason cited concluded that "pravastatin treatment alters the microarchitecture of aortic calcium deposits with potential effects on plaque stability". Specifically, mice given pravastatin had a greater total number of calcium deposits, but reduced overall calcium deposit surface area. This implies that statins increased the density of calcium deposits in the mice atheroclerotic plaques, and multiple studies in humans have found that "greater calcium density in plaques is associated with decreased CVD risk", due to a stabilisation effect of calcification on atherosclerotic plaque.
16:13: "Now this ties in with the most common cause of sudden heart attacks, which is not the presence of atherosclerotic plaques themselves but rather their rupture. High calcium scores indicate an increased tendency for plaques to rupture."
Again, Mason's claim is contradicted by the published medical literature:
"Several studies comparing acute heart disease with stable coronary heart disease (CHD) have shown denser calcified plaque in stable CHD.3-7 A recent study of CT angiography showed that the majority of individuals with CAC [coronary artery calcium] had calcified plaques, and that the CHD risk in this group was markedly lower than in patients with some or all plaques uncalcified.8"
Calcium Density of Coronary Artery Plaque and Risk of Incident Cardiovascular Events
High calcium scores do indicate a larger burden of atherosclerotic plaque, and hence a higher risk of an acute event resulting from plaque rupture. But the most heavily-calcified plaques are actually the least likely to rupture.
19:29: "Both high, and especially fluctuating, blood glucose levels generate oxidative stress at the level of the mitochondria, the consequences of which you saw earlier when combined with seed oil consumption, a very good reason to keep your blood glucose down."
High blood glucose levels, and the impaired insulin sensitivity that drives them, are undoubtably hazardous to your health. The problem for Mason's argument, is that studies consistently show that the polyunsaturated fatty acids found in "seed oils" lower blood glucose and improve insulin sensitivity, while saturated fats have the opposite effect. For example, a systematic review and meta-analysis of randomised controlled feeding trials found that:
"Replacing SFA [saturated fatty acids] with PUFA [polyunsaturated fatty acids] significantly lowered glucose, HbA1c [glycosylated haemoglobin, a measure of long-term average blood glucose levels], C-peptide [an indicator of how much insulin the body is making], and HOMA [homeostasis model assessment for insulin resistance]. Based on gold-standard acute insulin response in ten trials, PUFA significantly improved insulin secretion capacity (+0.5 pmol/L/min; 0.2, 0.8) whether replacing carbohydrate, SFA, or even MUFA."
And in this study conducted on abdominally obese individuals, 15 per cent of whom had diabetes, those assigned to eat a diet high in omega-6 fatty acids derived from vegetable oils (so-called "seed oils") had lower insulin and triglyceride levels than subjects assigned to a diet high in saturated fatty acids, derived from butter. Multiple markers of inflammation and oxidative stress were assessed, and "PUFA had no adverse effects on oxidative stress or inflammation; instead, n-6 PUFA may act as an anti-inflammatory, as evidenced by the reduced TNF-R2 and IL-1RA concentrations."
Mason's narrative that seed oils are the root of all evil, because they cause blood glucose dysregulation and oxidative stress, just isn't supported by the published literature.
20:26: "The consumption of seed oils began to rise in the early 1900s, well timed to have a causal role in the heart disease epidemic."
The graph shown by Mason to illustrate this claim was modified from a figure in this study. Here is the original, unmodified figure:
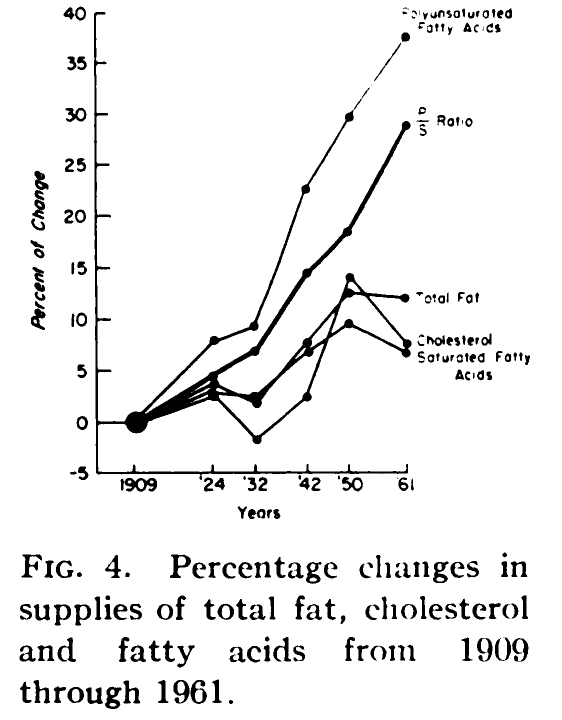
It does show a significant rise in the availability of polyunsaturated fats, doesn't it? But if we're going to play the 'correlation might indicate causation' game, why ignore this figure from the same study, which showed an even more precipitous decline in the availability of potatoes, grains and cereals, and other complex carbohydrates, and a massive surge in sugar supply, over the same time period?
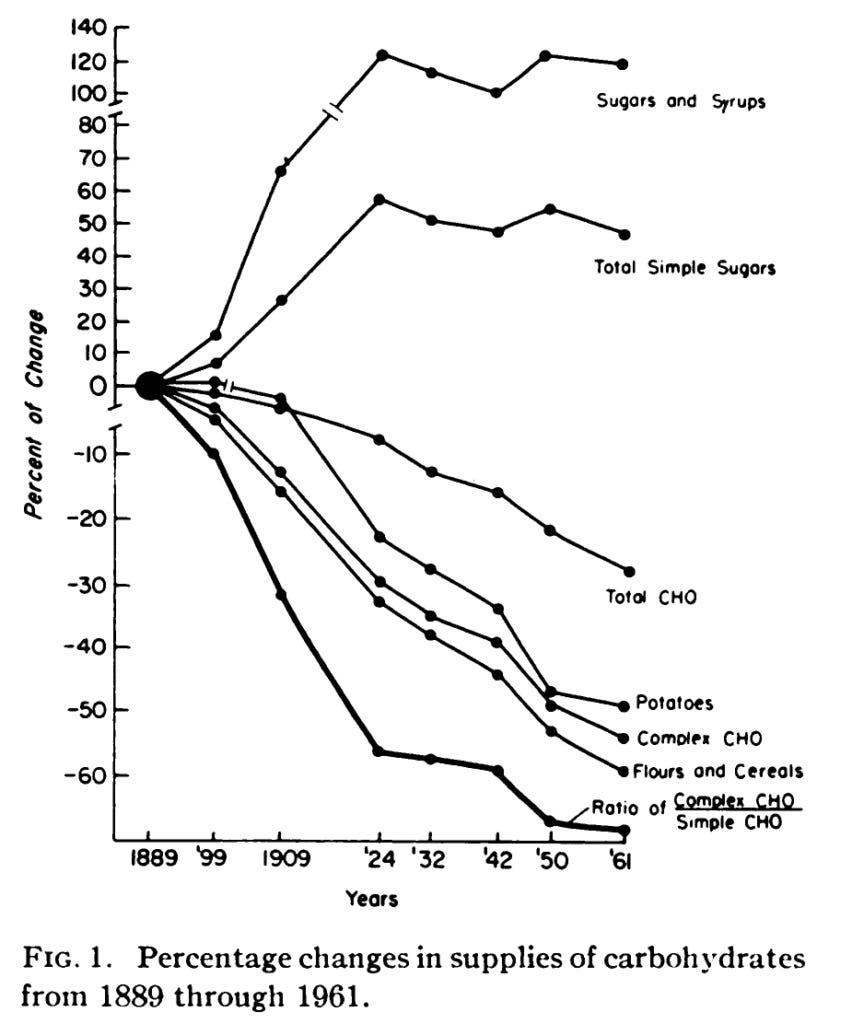
Because, once again, these data points don't fit with Mason's monomaniacal obsession with "seed oils".
20:35: "It's not just this association that suggests their consumption is problematic. Four randomised controlled trials, the gold standard of research have demonstrated the harm of consuming these seed oils."
The four trials that Mason referred to are this one, this one, this one and this one.
20:48: "In this study from 1965, patients post heart attacks were randomly allocated to one of three groups. There were two intervention groups consuming either olive or corn oil, also recommended to reduce their saturated fat intake, and a control group on a regular diet. After two years, 75 per cent of the subjects in the control group remained free of repeat heart attacks compared to 57 per cent and 52 per cent of the olive and corn oil groups respectively. Hardly a ringing endorsement for olive or corn oil. The conclusion of the investigators was quite blunt in fact: 'Corn oil cannot be recommended in the treatment of ischaemic heart disease'. And in my opinion the study also raises questions about olive oil."
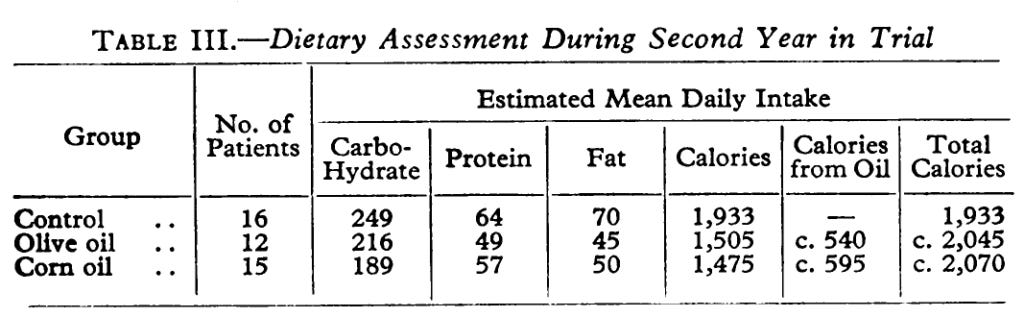
Mason's summary of the key findings of this study is accurate, although he neglected to mention that compliance with the prescribed treatments (80 g of either olive oil or corn oil, to be taken with meals in divided doses) was reasonably poor due to "distaste, nausea, and diarrhoea". Patients assigned to olive oil consumed, at most, 72.5 per cent of the prescribed dose, while those assigned to corn oil consumed a maximum of 80 per cent of the 80 g per day.
There were quite significant differences in macronutrient intake, with patients assigned to corn oil eating 25 per cent less carbohydrate than controls, for instance:
These differences in dietary intake, and their potential causes and impacts, were not discussed in the study.
21:38: "The Sydney Diet Heart Study was a randomised controlled trial examining the effects of replacing saturated fat with polyunsaturated fat, in men who had had heart attacks. But despite being finished in 1973, the results on whether this intervention reduced cardiac mortality were destined to never actually be published. It was only after Dr Chris Ramsden uncovered the raw data on punch cards and magnetic tapes, buried in a basement, that the full results were eventually published some 40 years later. The key finding being that the increased intake of polyunsaturated fats, as found in seed oils, increased the risk of death by 62 per cent."
This finding of a 62 per cent increase in all-cause mortality was indeed reported in the study, however Mason fails to include the 95 per cent confidence interval for this outcome, which was 1.00 to 2.64.
In statistics, the 95 per cent confidence interval indicates the level of uncertainty around the measure of effect. It represents "the range of values the true value in the population is expected to fall within based on the study results". The wider the confidence interval, the greater the uncertainty of effect. And
"If the 95% confidence interval of the RR or OR includes the value 1, that means it is possible the true value is 1 and there is no difference between groups. If that is the case, we say the null hypothesis cannot be rejected or that there is no statistically significant difference shown."
Again, translating that into English, the finding of a 62 per cent higher all cause mortality in this study is conceivably due to chance. The other reported outcomes had similarly wide confidence intervals, with the lower bound close to 1.
It's also important to point out that participants assigned to eat more polyunsaturated fat were instructed to replace saturated fats derived from animal fats, common margarines, and shortenings with safflower oil and safflower oil margarine. The 'Miracle' brand of margarine used in this study was a commercially-available product, and in the 1960s when this study commenced, it contained approximately 15 per cent trans fats. Trans fatty acids are well known to be extremely atherogenic even at low levels of intake, and to be "highly associated with the induction of inflammation, oxidative stress and lipoperoxidation".
To put it plainly, the Sydney Diet Heart Study was not a study examining the effects of replacing saturated fats with polyunsaturated fats, but of replacing saturated fats with trans fats plus polyunsaturated fats. It's hardly surprising that no benefits were observed from the consumption of fats that are known to be the most deleterious for cardiovascular health.
22:29: "A similar story exists for the Minnesota Coronary Experiment, which also finished in 1973... It was a double blinded randomised controlled trial on more than 9000 men and women, again evaluating the effect of increasing dietary polyunsaturated fats, and again there was an inexplicable delay in publishing the full findings. It took 16 years to just publish a few redacted findings, and when the results were finally published 43 years later, again after the raw data was located in a basement, it was revealed that increasing seed oil intake increased the risk of death, a result that was knowingly hidden for decades. And when the now deceased lead author was asked about this delay of publication, he explained it was because the study results were disappointing."
I discussed the Minnesota Coronary Experiment in an earlier article, so I'm going to save myself some time and simply quote myself:
"The Minnesota Coronary Experiment was originally intended to be a long-running intervention trial, in which dietary saturated fats (primarily from animal products) were almost entirely replaced with linoleic acid-rich corn oil. It enrolled residents of one nursing home and six state mental hospitals (9423 participants in total), a number close to the 10 000 participants that investigators had calculated would be required, in order to reach statistical significance.
However, the deinstitionalisation movement which resulted in the closure of many mental hospitals and discharge of long-term patients into the community, caused the failure of this study; almost three quarters of participants were lost within the first year and only about half of the remaining patients remained enrolled in the study for a full three years.With so few participants left, the study had no hope of reaching statistical significance."
There was little point in publishing the results of a study which could not be carried out according to its protocol. However, these results were
"published in 1989 in a paper titled 'Test of effect of lipid lowering by diet on cardiovascular risk. The Minnesota Coronary Survey', with frank acknowledgement that the study failed to show benefit of the intervention for cardiovascular events, cardiovascular deaths, or total mortality."
Specifically,
"For the entire study population, no differences between the treatment and control groups were observed for cardiovascular events, cardiovascular deaths, or total mortality. A favorable trend for all these end-points occurred in some younger age groups."
Test of Effect of Lipid Lowering by Diet on Cardiovascular Risk: The Minnesota Coronary Survey
Mason claims that a reevaluation of recovered data from the Minnesota Coronary Experiment, published in the BMJ in 2016, "revealed that increasing seed oil intake increased the risk of death". This is simply untrue:
"The BMJ article [i.e the reanalysis] states that there was ‘no mortality benefit for the intervention group in the full randomized cohort or for any prespecified subgroup’. In other words, there was no difference in outcomes. The finding of ‘22% higher risk of death for each 30 mg/dL (0.78 mmol/L) reduction in serum cholesterol’ applied equally to both the control and intervention groups, as is made clear on p. 9:
’In survival analyses (table 4), there was a robust association between decreasing serum cholesterol and increased risk of death, and this association did not differ between the intervention and control group (P>0.16 for all serum cholesterol×intervention interactions).’ [my emphasis]
Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968-73).
In other words, participants whose cholesterol levels fell the most over the course of the study were the most likely to die, regardless of whether they were in the dietary intervention group or the control group."
As I explained at length in my previous article, there is a "terminal decline" in cholesterol as people near the end of their lives:
"Declining cholesterol is the consequence of the deteriorating function that leads to death, rather than the cause of death. Anaemia, chronic inflammation, chronic renal and adrenal failure, nutrient deficiencies and hyperthyroidism (all common conditions in the final stages of life) all lead to reduced cholesterol production. Cancer, a leading cause of death, is also associated with reduced serum cholesterol, but cancer cells require cholesterol for growth and hence the relationship between low serum cholesterol levels and cancer is also attributable primarily to reverse causation."
I have been unable to locate any primary source for the claim that the study's lead author, Ivan Frantz, admitted that the study results were suppressed because they were "disappointing". If any reader could point me toward a source - such as an interview transcript, or recorded interview - please provide a link in the comments section below.
I'll reiterate the summary statement from my previous article:
"The final comment I would make on the Minnesota Coronary Experiment is that this study used an intervention (replacement of saturated fats with corn oil, much of it in foods that contained high levels of trans fats which are now known to be the most dangerous type of fats with regards to coronary artery disease) that is not advocated by any school of nutrition thought these days, so it has essentially no relevance to the modern 'diet wars'."
23:34: "More recently we've got the Women's Health Initiative study. So published first in 2006, it was a massive study of over 48,000 females designed to definitively assess the benefits of lowering saturated fat and increasing polyunsaturated fat intake. The most important outcome of this kind of study clearly being survival. And while the results were technically published, they were done in a very obscure manner, almost like the authors didn't want anyone to actually see them. This vague sentence on page 661 of the publication was the single reference to the only statistically significant finding within the whole paper. Remember this study cost US$700 million. And that was the best they could do. The finding being that females with a history of heart disease faced a 26 per cent increased risk of complications like heart attacks if they followed the intervention diet."
Once again, Mason fails to state the 95 per cent confidence interval of the "26 per cent increased risk of complications like heart attacks", which was 1.03-1.54 - in other words, it was barely statistically significant and hence, unworthy of being given prominence in the article.
Other findings which did not quite reach statistical significance were these:
"Compared with those in the entire comparison group, a trend was observed toward reduction of CHD risk among those in the intervention group who reached the lowest levels of saturated fat (HR, 0.81; 95% CI, 0.69-0.96 in the group that consumed <6.1% energy; P<.001 [adjusted HR, 0.82; 95% CI, 0.67-0.99; P = .05]) and trans fat (HR, 0.81; 95% CI, 0.69-0.95 in group consuming <1.1% energy intake; P<.001 [adjusted HR, 0.84; 95% CI, 0.69-1.02; P = .10]) or the highest intakes of vegetables and fruits (HR, 0.88; 95% CI, 0.76-1.03 in the group that consumed ≥6.5 servings/d; P<.001 [adjusted HR, 0.89; 95% CI, 0.74-1.06; P = .11])."
In other words, while most participants made very minor changes to their diets, the few who made more an effort appeared to be getting somewhat better results. Duh.
But far more importantly, Mason's statement that this study was "designed to definitively assess the benefits of lowering saturated fat and increasing polyunsaturated fat intake" is simply wrong. Here is the statement of intent from the study:
"The primary aim of the Women's Health Initiative (WHI) Dietary Modification Trial was to test whether behavioral intervention intended to produce a dietary pattern low in total fat [my emphasis], along with increased intakes of vegetables, fruits, and grains, would decrease the incidence of breast and colorectal cancer in postmenopausal women.15 A secondary aim was to test whether such a dietary intervention, which did not focus on the intake of specific fats [my emphasis], would also reduce the risk of CVD."
And from the Results section:
"By year 6, mean fat intake decreased by 8.2% of energy intake in the intervention vs the comparison group, with small decreases in saturated (2.9%), monounsaturated (3.3%), and polyunsaturated (1.5%) fat."
At this stage of my analysis of this presentation, I've run out of charitable instincts toward Dr Paul Mason. He is either incapable of reading a study abstract, or he's a bald-faced liar. In either case, anyone who trusts him to give evidence-based dietary advice - like the legions of adoring fans who populate the YouTube comments section on this video - is, quite frankly, seriously deficient in critical thinking skills.
25:11: "The problem is, we're consuming a huge amount of seed oils. This BMJ paper found that seed oil intakes exceeding 6 per cent of total energy are more harmful than high carb diets... The fact is, we would be much better off with animal fats."
This is the BMJ paper Mason was referring to. It did indeed find that once polyunsaturated fat intake - which is not all from "seed oils", since polyunsaturated fatty acids naturally occur in a wide range of foods, including animal products, all-cause mortality increased:
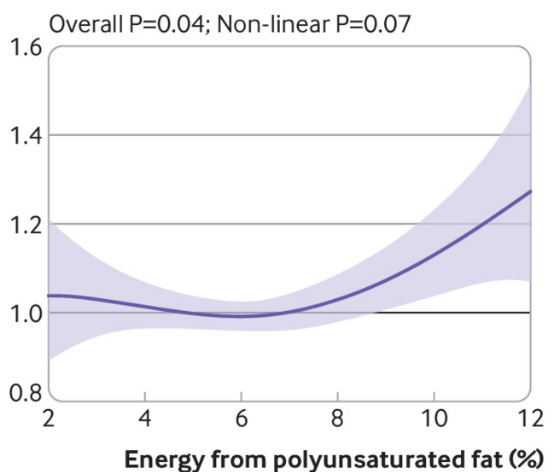
It also found that once intake of saturated fat - which is found mostly in animal fats - rose above 6 per cent, all-cause mortality rose at a very similar rate:
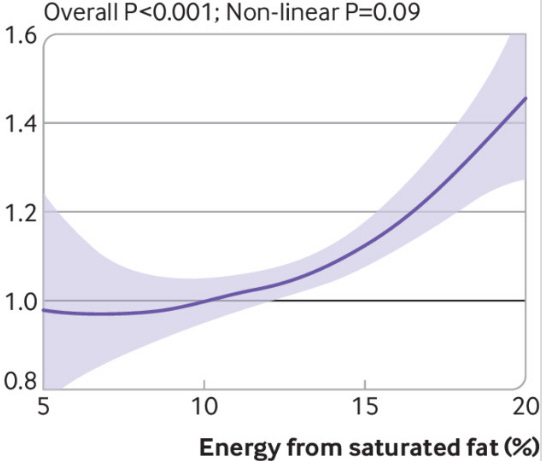
But strangely, Mason doesn't mention this finding, perhaps because it contradicts his conclusion that "we would be much better off with animal fats".
Here are some other studies that Mason, strangely, fails to mention:
A 2010 meta-analysis of eight randomised controlled trials, involving a total of 13,614 participants, which replaced saturated fat with polyunsaturated fat, found the following:
"The overall pooled risk reduction was 19% (RR = 0.81, 95% confidence interval [CI] 0.70–0.95, p = 0.008), corresponding to 10% reduced CHD risk (RR = 0.90, 95% CI = 0.83–0.97) for each 5% energy of increased PUFA, without evidence for statistical heterogeneity (Q-statistic p = 0.13; I2 = 37%). Meta-regression identified study duration as an independent determinant of risk reduction (p = 0.017), with studies of longer duration showing greater benefits."
If you'd prefer that in plain English, participants randomised to replace saturated with polyunsaturated fat lowered their risk of heart attack and/or cardiac death by 19 per cent compared to controls who continued their regular diet. Every 5 per cent extra increment of polyunsaturated fat intake lowered the risk of coronary heart disease by 10 per cent, and the longer people stayed on the intervention diet, the more benefits they got. The results of all the trials pointed in the same direction; that is, there were no trials in which the opposite finding (more CHD with higher polyunsaturated fat intake) was made.
An updated meta-analysis of intervention trials aimed at reducing saturated fat intake, published in 2020, found "a 21% (95% CI 0 to 38%) reduction in cardiovascular events in studies that replaced saturated fats by PUFAs". Note that the 95 per cent confidence interval includes 0, so it is possible that replacing saturated with polyunsaturated fat intake has no effect on cardiovascular events - which is still a far cry from blaming this substitution for causing such events, as Mason does.
Other studies have shown that linoleic acids and other omega-6 polyunsaturated fatty acids found in those dreaded "seed oils" do not cause inflammation; do not raise levels of lipid peroxidation products in humans, nor biomarkers of oxidative stress; but do reduce fasting insulin and enhance insulin sensitivity. Furthermore, higher blood levels of linoleic acid are associated with lower risks of total cardiovascular disease, cardiovascular mortality, and ischaemic stroke; and higher dietary intakes are associated with lower blood pressure.
And Mason discussed at length the processes that contribute to atherogenesis - adherence of LDL particles to the blood vessel wall, foam cell formation and secretion of matrix metalloprotease - and how he blamed them on "seed oil" consumption? Well, a study conducted in middle-aged, mostly overweight to obese volunteers found that overfeeding with saturated fat increased the aggregation of LDL particles. This aggregation ramps up the tendency of LDL particles to 'stick' to the inner lining of blood vessels, and promotes foam cell formation, and the secretion of matrix metalloprotease. On the other hand, overfeeding with unsaturated fats decreased binding of plasma lipoproteins to the proteoglycans found in the blood vessel wall.
In other words, higher intake of saturated fats ramps up multiple processes that lead to atherogenesis, while the unsaturatd fats have the opposite effect.
Although I initially baulked at the idea of wasting my extremely limited time on watching a video of Dr Paul Mason, I ended up finding the process of investigating his claims highly illuminating. His lecture was a masterclass in the skilled deployment of logical fallacies to persuade his audience that he is right about nutrition, and all the 'experts' are wrong.
After spending four intense days combing through every study cited by Mason, and many that he didn't cite because they contradict his assertions, I returned to the question that I posed in the subtitle of Part 1 of this article series: Is Dr Paul Mason a disruptive genius, a dissembling showman, or... something else?
My conclusion is that Mason knowingly and wilfully engages in deceptive conduct. Not only does he blatantly misrepresent, and selectively report, the findings of studies he cites, he also fails to mention the enormous body of research which contradicts his core assertion: that so-called "seed oils" are largely responsible for atherosclerotic heart disease. As to why he does this, I'm in no position to speculate.
Finally, I cannot stress the following point strongly enough: I do not personally recommend that you add omega 6-rich oils to your diet, or that you consume processed foods that contain them. Most people already eat more calories than they need, and oils are essentially empty calories, devoid of most micronutrients. And most processed foods that contain these oils are also full of highly refined carbohydrates, salt and food additives, whilst being deficient in fibre, unrefined carbohydrate and micronutrients. You cannot expect to attain or maintain good health if these foods constitute anything more than a tiny, occasional part of your diet. Instead of adding any kind of oil or fat to your diet, you should be focusing on consuming high quality, minimally processed, real foods.
However, blaming "seed oils" for the epidemic of chronic disease that's currently plaguing the entire developed world, and a good chunk of the developing world, is deceptive in the extreme.
All I can say is, if you base your dietary choices on the advice of people with as little respect for discovering truth as Dr Paul Mason, I wish you luck. You're going to need it.
If you appreciate my work, and would like to support me to do more in-depth critiques like this one, please consider a paid subscription to my Substack:




My speculation is Mason is another disinformation agent deflecting from the real culprit of rising diseases - THE INJECTIONS.
It is only speculation on my part, but based on the sheer volume and financial gains of agents pursuing their true craft.
Thank you so much for your intensive truthful work. I knew the entire "seed oil is deadly" thing was too coincidentally spread far and wide around 3 to 4 years ago.
Also, gotta love that name - "Mason". God Bless.
You wanted data that correlated what appears to be IR.
Roughly 15% increase in PUFA seems to cause a 15 point increase in bs, with no change in Insulin level. To me this looks like it. Clearly this a select group of individuals, but I doubt it's uniquely isolated. I'm surprised you have a question.