Part 2: The many faces of vitamin D... or, what doesn't vitamin D do?
As you'll (hopefully) recall from Part 1 of this miniseries, the substance that we call "vitamin D" is not in fact a vitamin, but a hormone - specifically, a sequence of three metabolites that culminates in a secosteroid hormone called calcitriol - which is synthesised from cholesterol through a multi-step process, that is set in motion when ultraviolet B (UVB) radiation from sunlight comes in direct contact with our skin.
Just to add a further wrinkle, we typically think of hormones as endocrine agents - that is, signalling molecules that are synthesised within one organ (the kidney, in the case of calcitriol), and then travel through the bloodstream to affect the activity of other organs. But vitamin D also acts as an intracrine and paracrine agent. That is, any cell can produce calcitriol from its precursor, 25-hydroxyvitamin D3, if it expresses the gene that codes for the enzyme 25-hydroxyvitamin D-1α-hydroxylase.
Cells with this capacity are located in, among other organs, the inner lining of blood vessels (endothelium), breast, prostate, parathyroid glands, muscles, placenta, brain, skin, and colon. Certain immune system cells also synthesise their own calcitriol. This locally-made calcitriol can be used to regulate the activity of the cell that produced it (intracrine) or that of neighbouring cells (paracrine).
A warning before I launch into describing the many activities of the sunshine hormone: Like Part 1, this post is going to go deep on detail. I'm not doing this just to nerd out (although I certainly do enjoy doing that!). I'm hoping to train you, my dear reader, to ask "why" and "how" questions. So many health claims are trotted out, both by conventional "authorities" and by self-styled gurus who make wild claims without providing any substantiating evidence - claims such as "vaccines have saved millions of lives", and "seed oils cause heart disease" and "lectins damage the gut" - and if you don't know anything about how the human immune system, or cardiovascular system, or gastrointestinal system actually work, you might be tempted to take these claims at face value.
The other motive for providing an explanation of how calcitriol exerts its activities in the human body, is that I want to draw your attention to how finely-regulated is the process of activating vitamin D and controlling its activities. As you read what follows, please keep this question in the back of your mind: "How would I go about determining how much vitamin D my body needs?" We'll return to that question in a later post in this miniseries.
Throughout this post, I will use the terms "vitamin D" and "calcitriol" more or less interchangeably; remember that whenever you see any biological action attributed to "vitamin D", that action can in fact only be carried out by the fully activated version of the substance, calcitriol, or 1,25-dihydroxyvitamin D3. Although most studies that examine vitamin D status as a risk factor for disease, refer to the circulating, inactive precursor to the hormone calcitriol as "vitamin D", I will disambiguate by specifying this, correctly, as 25-hydroxyvitamin D.
What does vitamin D the hormone calcitriol do?
As with other hormones, vitamin D/calcitriol exerts its biological activity by interacting with receptors, which are located in cells that comprise its target organs. Virtually every tissue and cell in the body - including the heart, stomach, pancreas, brain, skin, gonads, and immune system cells - has vitamin D receptors (VDR), meaning that pretty much every organ is a target organ for this hormone.
Once these vitamin D receptors have been activated by binding with either circulating or locally-made calcitriol, specific genes that regulate metabolic processes are switched on or off. Calcitriol controls the activity of at least 220 genes that are involved in regulating a wide variety of biological processes, and over 2700 sites of VDR binding have been identified in the human genome, with a particularly high concentration of binding sites in the vicinity of genes associated with autoimmune diseases and cancer.
Dem bones, dem bones
The most well-known function of vitamin D, and its primary endocrine function, is its role in the regulation of calcium and phosphate metabolism, which profoundly impacts bone development and integrity. This regulation is exerted via three actions: increased absorption of dietary calcium and phosphorus, decreased loss of calcium and increased loss of phosphorus in the urine, and breakdown of bone to release calcium and phosphorus.
The binding of calcitriol to vitamin D receptors within the cells lining the small intestine, increases the absorption of dietary calcium, by boosting the amount of calcium that these cells actively take up from the contents of the gut (transcellular absorption), as well as facilitating the passive diffusion of calcium between these cells (paracellular absorption). Calcitriol's effects on calcium absorption are profound:
"Without vitamin D, the small intestine absorbs no more than 10-15% of dietary calcium. In a person with vitamin D sufficiency, the small intestine absorbs, on average, 30% of dietary calcium; during growth, lactation, and pregnancy, the efficiency increases to 80%."1
Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis
Likewise, without vitamin D, only about 60 per cent of dietary phosphorus is absorbed, while adequate vitamin D boosts the absorption rate to 80 per cent.
Maintaining a fairly constant level of calcium in the bloodstream is vitally important for muscle contraction, including the heart muscle. If the blood level of calcium drops, the parathyroid glands begin to secrete parathyroid hormone, which causes the kidneys to recapture calcium that was on its way to being excreted via urine, and to put it back into circulation.
Parathyroid hormone also causes the bones to release some of their calcium in order to top up the blood level of this vital mineral. This calcium is released in the form of calcium phosphate, and parathyroid hormone increases the loss of phosphorus via urine.
And finally, parathyroid hormone stimulates the kidneys to produce calcitriol, to boost intestinal calcium absorption as described above.
The body has three major mechanisms for keeping calcitriol levels in check:
As calcitriol levels rise, parathyroid hormone release is suppressed, preventing excess formation of calcitriol.
High serum calcium and phosphorus levels also suppress calcitriol production.
Calcitriol triggers production of the enzyme that causes its breakdown, as well as that of its precursor, 25-hydroxyvitamin D.
If vitamin D deficiency occurs during skeletal development, in utero and/or during childhood, there may be insufficient calcium phosphate available to fully mineralise the bones, leading to the bone deforming and growth retarding disease, rickets2.
Prolonged vitamin D deficiency in adulthood causes osteomalacia, a painful condition of bone demineralisation and softening, in which the protein matrix of the bone is preserved. Osteoporosis, which is characterised by loss of both the bone matrix and minerals, may be precipitated and exacerbated by the secondary hyperparathyroidism that accompanies prolonged vitamin D deficiency, although typically only mild to moderate deficiency of 25-hydroxyvitamin D is seen in osteoporotic patients. Both osteomalacia and osteoporosis increase the risk of bone fracture.
What's good for bones is good for teeth
The process of tooth mineralisation occurs in parallel to skeletal mineralisation, and insufficient vitamin D has similar effects: "the 'rachitic tooth', which is a defective and hypomineralized organ highly susceptible to fracture and decay." In addition, the cells that build enamel and dentin are highly reliant on proteins that are only constructed when the vitamin D receptor binds to calcitriol.
If a pregnant woman is deficient in vitamin D during critical phases of gestation, her baby can be born with overly small and undermineralised teeth, and enamel defects.
Aside from the involvement of vitamin D in tooth mineralisation, as far back as the 1920s and 30s, it was observed that people with higher UVB exposure due to geographic location had a lower risk of dental caries (cavities), and subsequent research has confirmed that vitamin D mediates this protection against tooth decay. When the vitamin D receptor binds to calcitriol, two antimicrobial peptides (small proteins), cathelicidin and defensins, are induced (more on this below). Cathelicidin and defensins both attack bacteria that are linked to dental caries, as well as to periodontitis (gum disease, the major cause of adult tooth loss).
Immunomodulation - getting the balance right
Calcitriol plays a critical role in the immune system's defensive activities. When front-line immune cells known as monocytes and macrophages encounter potentially dangerous bacteria or one of their components, lipopolysaccharide (also known as endotoxin), they switch on their own vitamin D receptor gene, and they ratchet up their own production of calcitriol from circulating 25-hydroxyvitamin D. The increased calcitriol facilitates synthesis of cathelicidin which, as mentioned above in the discussion of dental health, is capable of destroying some infectious agents - including Mycobacterium tuberculosis, the organism associated with tuberculosis3, and Helicobacter pylori, which is associated with gastritis.
Furthermore, the calcitriol produced by monocytes and macrophages has paracrine activities which modulate the defensive capabilities of other types of immune cells, including the T lymphocytes that directly attack infectious agents, and the B lymphocytes which release antibodies to destroy infectious agents.
At the same time as it ramps up the production of antimicrobial peptides and neutralising antibodies, calcitriol also tamps down the production of inflammatory cytokines, reducing inflammation and oxidative stress, while upregulating production of anti-inflammatory cytokines and preventing overproduction of antibodies (which can lead to autoimmunity).
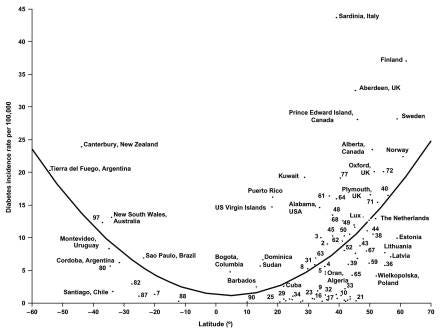
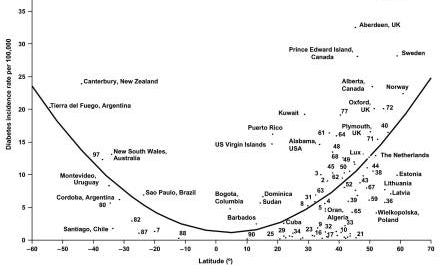
Thus, not only does calcitriol help to clear infections, it's also vital for preventing autoimmune diseases - a broad group of conditions in which the immune system attacks the body's own cells and tissues. As you'll recall from Part 1, UVB exposure is highest at the equator and drops off with increasing latitude; with decreased UVB exposure there is diminished capacity to produce vitamin D from solar irradiation of the skin. Living at higher latitudes increases the risk of a number of autoimmune diseases including type 1 diabetes, multiple sclerosis, rheumatoid arthritis, ulcerative colitis and Crohn’s disease.
High circulating levels of 25-hydroxyvitamin D are associated with a lower risk of multiple sclerosis, with the protective effect especially strong when measured before the age of 20.
Anticancer activities
Calcitriol regulates a number of genes that are absolutely critical to the development of cancer, including some that control cell division, differentiation of cells, apoptosis (programmed cell death) and angiogenesis (the growth of new blood vessels, which is critical for tissue healing but also for tumour growth).
As far back as 1916, an insurance statistician observed that globally, the cancer death rate is higher in regions further from the equator. This finding was confirmed in the US population in the 1940s.
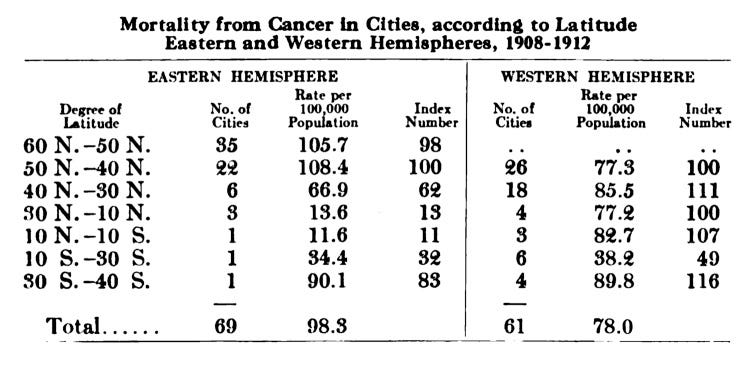
Both the incidence of, and mortality from, cancer of the bladder, breast, cervix, colon, endometrium, oesophagus, stomach, lung, ovary, prostate, pancreas, rectum, kidney and vulva, as well as both Hodgkin’s and non-Hodgkin's lymphoma, have been found to be higher in people living in higher latitudes than in people living at lower latitudes. And, as I wrote in Skin cancer checks: life-saver or scam? (and further confirmed in this study, higher sun exposure is associated with decreased risk of developing a fatal melanoma.
Low circulating levels of 25-hydroxyvitamin D have been associated with increased risk of colorectal cancer.
Muscling up on sunshine
Skeletal muscles have a VDR, and calcitriol plays a crucial role in muscle growth, maintenance, contraction and repair. Muscles may even serve as a dynamic depot for vitamin D, helping to maintain circulating 25‐hydroxyvitamin D levels during periods of low sun exposure.
Severe vitamin D deficiency results in muscle weakness, and 25-hydroxyvitamin D status is a predictor of muscle strength and performance in older adults.
Calcitriol also increases the strength of contraction of the heart muscle.
Cardiometabolic effects
The insulin-secreting beta cells of the pancreas have a VDR, and calcitriol is a potent stimulator of insulin secretion.
Calcitriol produced in the kidney inhibits the secretion of renin, an enzyme which sets in motion a cascade of hormonal effects that leads to higher blood pressure.
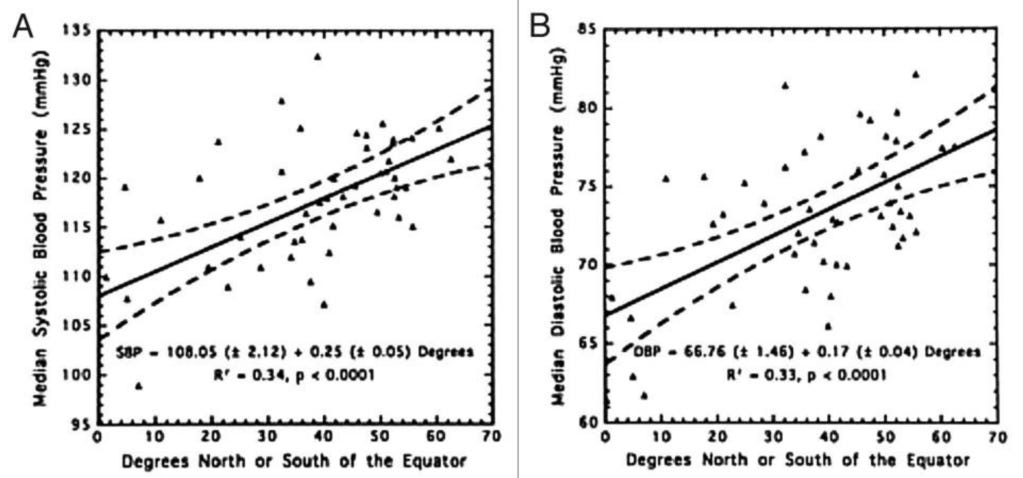
Finally, low 25-hydroxyvitamin D levels have been associated with increased risk of heart attack, and especially fatal heart attack.
Neurological effects
Cells in the human brain not only express the VDR but also produce the enzyme that synthesises calcitriol from circulating 25-hydroxyvitamin D. Calcitriol may increase serotonin levels, and it has been shown to stimulate clearance of amyloid-β, the waste product whose accumulation within the brain is associated with Alzheimer's disease.
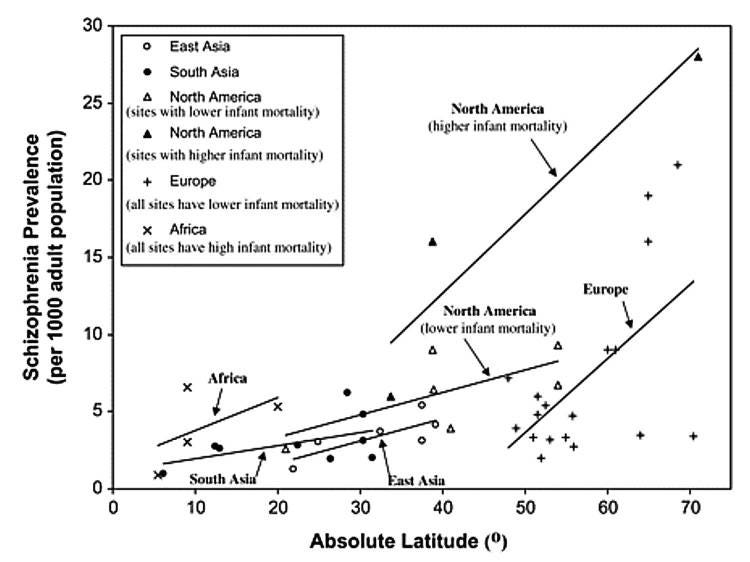
The prevalence of schizophrenia is higher in regions with higher latitude, and babies born in winter have a higher risk of developing schizophrenia later in life.
Multiple studies have found lower circulating levels of 25-hydroxyvitamin D in depressed adults.
Conclusion
Vitamin D/secosteroid calcitriol is a hormone which regulates a multitude of biological processes that maintain and restore health. Virtually every tissue and organ in the body has receptors for calcitriol, and many have the capacity to make their own, from circulating 25-hydroxyvitamin D.
The striking association between higher latitude and prevalence of many chronic diseases - from type 1 diabetes and multiple sclerosis to hypertension and schizophrenia - underlines the importance of UVB exposure to human health.
But is it possible to compensate for suboptimal UVB exposure by supplementing with "vitamin D" (more accurately, with cholecalciferol and/or ergocalciferol), and if so, what is the optimal level of 25-hydroxyvitamin D that we should be aiming for? The answers to those questions are far from straightforward, but I'll be diving into these murky waters in the next post.
As always, I look forward to reading your thoughts and reflections:
And finally, this post has taken me approximately 20 hours to research and write (and I’m still only just getting started on this vitamin D deep dive!). I make all my posts freely available to all readers, because I believe we all deserve access to information that helps us to take greater control over our health. But I rely on my small core of paid subscribers to provide this service to those who genuinely can’t afford it.
Isn't it cool that a pregnant woman's body simply absorbs more calcium from her diet, as required, in order to build her baby? As long as she is getting enough UVB exposure and eating a diet of nutritious foods, she doesn't need to intentionally increase her intake of calcium.
One of the consequences of rickets is pelvic deformation and narrowing of the pelvic outlet. In females, this decreases the likelihood of carrying a pregnancy to full term and giving birth to a live infant. This is an excellent example of the phenomenon that evolutionary biologists call selection pressure. Women who can't reproduce don't pass on their genes. So if a particular woman has a mutation in the genes that control melanin production, which results in a lighter skin shade that allows her to produce more vitamin D from limited sunlight exposure in a higher latitude, she is more likely to have good skeletal development which will allow her to have more offspring than a darker-skinned woman in that same environment. Her children will inherit half of her genome, so at least some of them will be lighter-skinned like their mother. Her paler daughters will be more reproductively successful, and her paler sons will pass on the genes that code for less melanin to their daughters, increasing their chances of reproductive success. This is what is meant by "survival of the fittest" - not a dog-eat-dog competition for scarce resources, as it is often mischaracterised, but the enhanced reproductive success of those whose genes confer the best "fit" for the particular environment in which they currently operate.
Before the discovery of antibiotics, the most successful treatment regime for tuberculosis was heliotherapy - the deliberate exposure of tuberculosis patients to sunlight.



Any info of best form of vitamin D?
That was a very informative great post. Thank you!