New study finds all forms of hormonal contraception raise breast cancer risk
Messing with women’s biology has consequences
Ever since the first oral contraceptive was approved in 1960, ‘The Pill’ has been hailed as a liberator of women. It granted to women, for the first time in history, the ability to exercise control over their reproductive function. Initially, the oral contraceptive pill was only made available to married women, allowing them to decide when, and if, to have children. In 1965, this restriction was lifted and doctors were permitted to prescribe the Pill to any woman, married or single, who asked for it.
The advent of reliable contraception that was controlled (at least at the user end) by women, ushered in unprecedented social change. Women’s mass-scale entry into the workplace set off a chain of events that culminated in significant legislative changes including anti-discrimination laws and guarantees of equal pay for equal work, as well as a profound transformation in attitudes towards women’s capabilities and role in society.
And of course, the sexual revolution of the swinging 60s would not have been possible without the fear of unwanted pregnancy having been effectively nullified by the Pill. For the first time ever, women could engage in casual sex, or premarital sex, without risking an unwanted pregnancy which might force to choose between a shotgun wedding with a man they didn’t really love or barely knew, a potentially lethal ‘backyard’ abortion, or being ‘sent to the country’ to give birth to a baby who would immediately be given up for adoption (which is how my older brother and sister came into my parents’ care). Conversely, single motherhood was significantly destigmatised, and it became an economically feasible alternative to surrendering one’s child for adoption with the introduction of social welfare programs such as the Single Mother’s Benefit implemented by Gough Whitlam, possibly Australia’s most polarising Prime Minister.
In fact, it’s virtually impossible for those of us who have grown up in the post-Pill era, to imagine living in a world that had not been utterly transformed by hormonal contraception.
But any economist, and any evolutionary biologist, will tell you that life is always and everywhere a series of trade-offs, not a steady march toward perfection. Every ostensible advancement or improvement has costs, which may not be immediately apparent.
A new generation of feminist authors, including Mary Harrington and Louise Perry, have made forceful arguments that the Pill-fuelled sexual revolution has been harmful to the happiness of both men and women, and to the well-being of children.
Perry provocatively asserts that the easy availability of oral contraception caused women to lose, rather than gain, sexual agency in that they could no longer use the fear of unwanted pregnancy to deny men casual sex. Harrington is particularly concerned about the commodification of sex that inevitably occurs when it is decoupled from its biological function of reproduction:
Quite aside from the profound psychosocial and cultural impacts of readily-available and reliable contraception, the Pill and its spin-offs – including implants and progestagen-releasing intrauterine devices (such as Mirena) – are like any other medicine: they have side effects.
Previously, I’ve written about the impact of hormonal contraception on women’s risk of anxiety and depression. In Hormonal contraception and women’s mental health, I shared the results of a massive Danish study which found that women using any form of hormonal contraception (including oral contraceptive pills, patches, vaginal rings and hormone-releasing IUDs) were more likely to be diagnosed with depression. Compared with women who used no form of hormonal contraception, the risk of being prescribed antidepressants for the first time ranged between 23 per cent higher for women taking the combined oral contraceptive pill, to 100 per cent higher (i.e. a doubling of risk) in women using a contraceptive patch.
The Danish study also found that the risk was even higher in adolescents, with girls aged 15-19 being 80 per cent more likely to be diagnosed with depression if they were taking the combined oral contraceptive pill, all the way up to three times more likely if they used non-oral hormonal contraceptives (again, including the ever-more-widely prescribed Mirena).
In More evidence that taking the Pill in your teens is linked to depression, I reported US data that confirmed the Danish study, finding that women who had never used oral contraceptives had less than one third the odds of suffering major depression as women who had started taking the Pill during adolescence.
Then, in This is your brain on the Pill, I delved into two studies which identified distinct changes in the structure and function of the brains of women taking oral contraceptives. Namely, Pill-taking women had significantly smaller volume of the hypothalamus, a region of the brain that produces many hormones and helps regulate essential bodily functions including body temperature, mood, appetite, sex drive, sleep cycles and heart rate. They were more reactive to emotionally negative images, and those who had begun taking oral contraceptives in adolescence also showed a blunted response to a social stressor, which has previously been found to be a risk factor for depression.
And in How the Pill and HRT affect your gut… and your risk of autoimmune and inflammatory disease, I summarised multiple studies which found that women taking oral contraceptives are at higher risk of inflammatory bowel disease (Crohn’s disease and ulcerative colitis), multiple sclerosis, systemic lupus erythematosus and interstitial cystitis.
But as devastating as anxiety, depression and autoimmune conditions are, both for those who suffer them, and their loved ones, the disease that women have been conditioned to fear more than any other is breast cancer.1
It has long been acknowledged that both current and recent use of combined oral contraceptives (containing synthetic versions of the hormones oestrogen and progesterone, the latter known as progestagens) are associated with an increased risk of developing breast cancer.
Since oestrogen is required for the growth of the most common form of breast cancer, there was initially some cautious optimism that progestagen-only contraceptives might be a breast-safe option. But a study of nearly 28 000 UK women, published in March 2023, has poured cold water on that hope.
The study, ‘Combined and progestagen-only hormonal contraceptives and breast cancer risk: A UK nested case–control study and meta-analysis’, used the Clinical Practice Research Datalink (CPRD), a computerised UK primary care database containing anonymised, linked, and prospective medical records for approximately 11 million individuals registered with a National Health Service (NHS) general practitioner (GP), to examine the relationship between breast cancer and the use of any form of hormonal contraception. Researchers identified 9498 women aged between 20 and 49 years who were enrolled in the CPRD, were diagnosed with invasive breast cancer between 1 January 1996 and 20 September 2017, and had received one or more prescriptions for any form of hormonal contraception between 1 January 1995 and their date of diagnosis. Two controls – women who were not diagnosed with breast cancer during the study period – were selected for each woman with a breast cancer diagnosis; these controls were matched for age, GP practice and length of observation period.
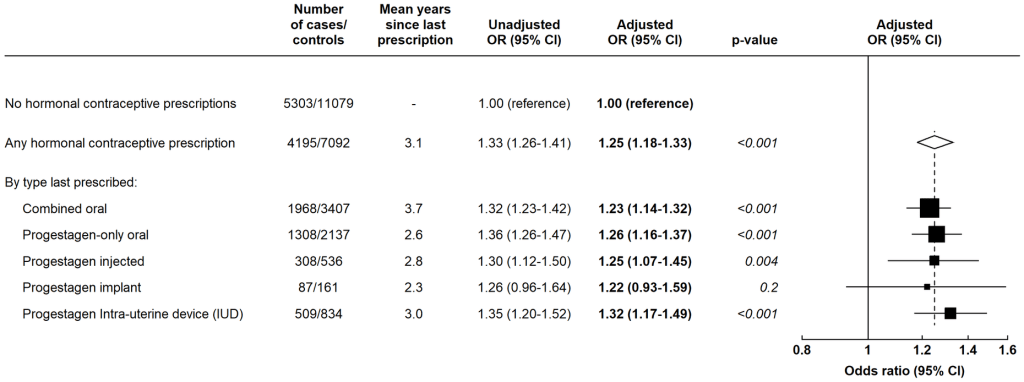
When the researchers compared contraceptive use in the cases vs controls, they found that use of all forms of hormonal contraception were associated with an increased risk of developing breast cancer.
Specifically,
Women who had used the combined oral contraceptive (oestrogen + progestagen) at any point during the observation period had a 23 per cent higher risk of being diagnosed with breast cancer than women with no use of hormonal contraceptive;
Women who took an oral progestagen-only contraceptive pill had a 26 per cent higher risk;
Women who used an injectable progestagen had a 25 per cent higher risk;
Women who used a progestagen IUD (Mirena) had a 32 per higher risk.
Too few women used a progestagen implant for the researchers to calculate risk accurately.
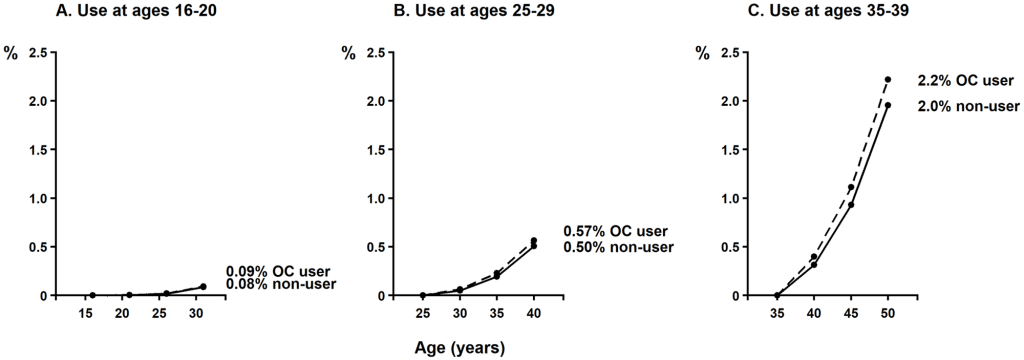
It’s important to point out that the increase in absolute risk of breast cancer associated with use of hormonal contraceptives is small:
For women who used any oral contraception between the ages of 16 and 20, an additional 8 per 100,000 users will develop breast cancer over the course of 15 years, on top of the base rate of breast cancer (an increase in incidence from 0.084% to 0.093%).
For women who used oral contraception between 25 and 29, 15 year excess risk is about 61 per 100,000 users (from 0.50% to 0.57%).
For women using oral contraception between 35 and 39, 15 year excess risk is about 265 per 100,000 users (from 2.0% to 2.2%).
However, having seen many clients who have gone through the painful, humiliating and disfiguring process of breast cancer treatment, I think most would tell you that if they had known of anything that might have reduced their risk of this horrendous experience even a little, they would have jumped at it.
Assessment of risk is in the eye of the beholder. In my personal and professional experience, the vast majority of doctors do not even mention the potential side effects of hormonal contraceptives that they prescribe. A woman cannot give informed consent if she is not apprised of all the risks of treatment.
Furthermore, I see many women – including adolescents and young women – who suffer from painful or heavy periods, or menstrual irregularity. Almost all of them report that their GP prescribed either an oral contraceptive or progestagen-releasing IUD, without any discussion of potential adverse effects, and without even a rudimentary investigation of potential underlying drivers of their menstrual disorders.
Just as hormonal contraception made it easy for men to get sex without having to put the work into courtship and proving themselves worthy of marriage, it has facilitated lazy doctoring. Why bother putting the work into investigating why a woman is suffering from painful or irregular periods, or educating her about the diet and lifestyle habits which contribute to menstrual dysfunction, when you can just put her on the Pill to ‘regulate her cycle’ (which is arrant nonsense, as hormonal contraceptives disrupt the delicate orchestration of the reproductive cycle), or insert a Merina which has a one in five chance of stopping her from menstruating altogether? Voila – problem solved… or more to the point, neatly concealed.
It’s a sad state of affairs when it is considered perfectly acceptable to put girls and women at increased risk of mental health disorders, autoimmune conditions and breast cancer by prescribing hormonal contraceptives that profoundly impact their physiology, while not only depriving them of informed consent, but also failing to address the diet and lifestyle behaviours and underlying health issues that are causing their current symptoms, and are likely to generate more and more serious disorders as time goes by.
It’s been over 60 years since the Pill launched a cultural, social, economic and sexual revolution. Hormonal contraception has also been embraced enthusiastically as a therapeutic option, by the vast majority of doctors. But it’s high time we paused to carry out an honest accounting of its effects, for good and ill. For many women, the costs of hormonal contraception just aren’t worth it.
For information on my private practice, please visit Empower Total Health. I am a Certified Lifestyle Medicine Practitioner, with an ND, GDCouns, BHSc(Hons) and Fellowship of the Australasian Society of Lifestyle Medicine.
Breast cancer is only the fifth leading cause of death in Australian women. Almost three times as many women die of dementia, and more than twice as many die of coronary heart disease, as die of breast cancer.




So we've got contraceptives causing cancer, statins causing Alzheimers and dementia, vaccines causing cancer, autism, allergies... what diseases are left that arent iatrogenic?
Great post!
I used the combo OCP for only 3 weeks when I was 20. It made me so sick, I had to take an anti-nausea tablet to cope! I remember when that anti-nausea tablet wore off and I thought I was going to puke on the desk at Uni! I went to the bathroom, somehow managed to not throw up, and said to myself "No more pill. Ever." And I've stuck to it!
The more I read about the OCP (in whatever form), the more problems I find related to it! Horrible things!
Interesting that the use of those nasty Mirenas have the highest increase risk of breast cancer. They have been pushed so much in recent years, with so many women allowing themselves to have them inserted! Urgh!
I honestly wonder why women subject themselves to these invasive procedures, or taking all sorts of chemicals with all sorts of negative long-term problems (which they're never told about by the way), just so they don't get pregnant? Then later on their 30s they clamour that they can't get pregnant, and many use IVF! I mean, it's such a stupid situation! And anyway, there's never a 'good time' to have a kid. It can always a bit tricky no matter when you have one! :-D
But it seems a really weird idea to spend so much time, energy and danger to NOT get pregnant, all so one can have the autonomy to say "I want a kid...NOW" later on. And invariably with environmental/genetic toxic build-up, that still doesn't happen anyway!
The snake-oil salesmen never went out of business, did they?! :-D