The latest depressing news on antidepressant drugs
The evidence against antidepressant drugs just keeps piling up.
Long-time subscribers of my EMPOWERED! newsletter will know that I have a particular interest in antidepressant medications – specifically, their lack of efficacy, their laundry list of side effects, the utter fraudulence of the ‘biochemical imbalance’ theory of depression which buttresses their use, and the disease-mongering and diagnostic bracket-creep that pharmaceutical companies have engaged in, to hoodwink doctors into prescribing them for people who are undergoing perfectly normal emotional reactions to challenging life circumstances.
If you’re interested in exploring my previous articles on this topic, here they are:
‘Depressed’ or just going through a rough patch – have you been misdiagnosed?
More elderly people are taking antidepressants, but they’re just as depressed
Antidepressant discontinuation syndrome – an underrecognised and rapidly escalating problem
A reader’s response to ‘5 reasons to think twice before taking an antidepressant’
The biochemical imbalance theory is dead. Someone should tell your doctor
Why do I have such a bee in my bonnet about these medications? Firstly, a high percentage of my clients (especially females, who make up the majority of my clientele) are either on antidepressants when they come to see me, or have been in the past. Most were prescribed these potent neurotoxic chemicals merely because they were experiencing perfectly understandable distress due to various forms of loss. In one particularly memorable case, a client reported to me that her GP had prescribed antidepressants after her beloved dog died, in case she felt overly sad. (To her great credit, the client threw the prescription in the bin on her way out.)
Secondly, many of the physical and psychological symptoms my clients present with are directly attributable to the effects of antidepressant drugs, although this fact has rarely been acknowledged by their doctor/s, for reasons explained with exceptional clarity and incisiveness in a four-part series on A Midwestern Doctor’s Substack (see links to the series, which is on medical injuries more generally, but is highly relevant to psychotropic-induced injuries, at the bottom of this post).
And thirdly, as a practitioner I find that antidepressants both indirectly and directly undermine my therapeutic approach, which is founded on empowering individuals to take charge of their own health.
The indirect undermining effect is mediated by the narrative promoted by the medical-industrial complex, which is that the complex of psychological and physical effects characterised as depression is a ‘mental illness’ – a profoundly disempowering framing. I view depression through an evolutionary lens, as an adaptive behaviour that evolved to keep people focused on the source of their distress until they come up with a solution to resolve the relevant problem. Framing depression as an intensely painful but adaptive experience, from which individuals can and do emerge thriving, is deeply empowering.
The direct undermining effect is mediated by the apathy these drugs induce in people who take them. As one client described it to me, “When I was taking those drugs, I didn’t feel really sad, or really anxious, but I also didn’t feel really happy. I just didn’t feel much of anything at all.” This numbing effect of antidepressants was wonderfully satirised by the incomparable Robin Williams – who at the time of his death by suicide was taking an antidepressant called mirtazapine, which carries a black box warning that it may increase suicidal thoughts or actions – in his ‘Fukitol’ stand-up routine (warning for the easily-offended – naughty language ahead):
As the manufactured COVID crisis has been occupying so much of my research and writing time, a rather large list of antidepressant-related publications has accumulated in my “ideas for articles” file. While each of them could easily be the subject of an entire post, when considered all together, they form quite a interesting picture. I’ll summarise each of them briefly and then discuss the implications, as I see them.
1. Antidepressants and health-related quality of life (HRQoL) for patients with depression: Analysis of the medical expenditure panel survey from the United States
This study, published in PLOS [Public Library of Science] One, used the United States’ Medical Expenditures Panel Survey (a nationally representative database) to identify all patients who were diagnosed with depression – on average, a startling 17.47 million adult patients per year – and then to track their health-related quality of life over time, comparing outcomes in those who were prescribed antidepressants with those who weren’t.
Roughly 58 per cent of all those with a depression diagnosis were prescribed antidepressants, with more women (60.5%) than men (51.5%), and more white and Native American than black, Asian, Hawaiian native or Pacific Islander people leaving their doctor’s office with a script. Interestingly, people who had never been married were less likely to be prescribed antidepressants than those who were, or had been, married.
All participants completed questionnaires at regular intervals, that assessed both the physical and mental dimensions of their health-related quality of life. These questionnaires are classified as patient reported outcome (PRO) measures, in contrast to the standard questionnaires that doctors use to screen patients for depression and anxiety (the PHQ-9 and GAD-7) respectively, and to assess change in symptoms over time. As I wrote in Who says you’re depressed or anxious? Pfizer does, both the PHQ-9 and GAD-7 were developed by academics funded entirely by the pharmaceutical giant Pfizer, and Pfizer owns the intellectual property and is responsible for distributing the PHQ-9 and GAD-7 to doctors – clearly because the symptoms that these instruments focus on are those most likely to change when patients are prescribed one of Pfizer’s top-selling psychoactive drugs, which include venlafaxine (Efexor), sertraline (Zoloft), escitalopram (Lexapro) and alprazolam (Xanax).
However, as the authors of this study point out,
“PRO measures are good indicators that can be utilized in this case because improving patients’ outcomes are the ultimate goal of therapy.”
What a novel concept – the ultimate aim of treatment is to improve patient outcomes, rather than Big Pharma’s bottom line.
Participants were asked a series of questions broken down into a physical component summary (PCS) and mental component summary (MCS). The former assessed physical functioning, role limitations due to physical health problems, bodily pain, general health, and vitality (energy/fatigue); and the latter evaluated social functioning, role limitations due to emotional problems, and mental health (psychological distress and psychological well-being).
The researchers then looked at whether depressed people who took antidepressants showed a greater improvement on either the physical or mental components of health-related quality of life than those who didn’t take any medication.
And – drum roll please – they didn’t.
Both groups improved slightly on the mental component summary, and there was no difference between the degree of improvement experienced by depressed people who were taking antidepressants compared to those who weren’t. And if anything, more people who weren’t taking antidepressants improved slightly more on the physical component summary than those were taking drugs.
The authors concluded:
“The ultimate goal of using antidepressant medications or psychotherapy is to improve patients’ important outcomes, such as HRQoL. The real-world effect of using antidepressant medications does not continue to improve patients’ HRQoL over time, as the change in HRQoL was comparable to patients who did not use any antidepressant medications.”
They also set their findings into the context of the broader literature on antidepressants:
“Patients who were receiving either placebo or psychotherapy showed lower relapse rate than those who were on antidepressant medications [43]. These results, to some extent, coincide with the results of this study as the use of antidepressant medications was associated with higher rate of relapse compared to placebo, which makes the continuous prescribing of antidepressant medications a matter of preference rather than a necessity.”
2. Association of Selective Serotonin Reuptake Inhibitor Use With Abnormal Physical Movement Patterns as Detected Using a Piezoelectric Accelerometer and Deep Learning in a Nationally Representative Sample of Noninstitutionalized Persons in the US
Digging deeper into the effect of antidepressants on physical functioning, this study examined the effect of the most commonly-prescribed class, selective serotonin reuptake inhibitors (SSRIs) on intensity of body movement in a cross-sectional sample of 7162 participants from the 2005-2006 National Health and Nutrition Examination Survey (NHANES), a nationally representative population-based sample of noninstitutionalised persons in the US.
Participants wore a piezoelectric accelerometer (a type of movement tracker, like a FitBit) on their right hip for at least one week, and the movement data gathered by the device was then compared between participants who were, and were not, taking SSRIs.
Overall, those taking SSRIs moved less. They also showed a slower morning increase in movement and a slower evening decrease in movement than participants who were not taking these drugs, suggesting that the drugs were disrupting their sleep architecture and exacerbating insomnia.
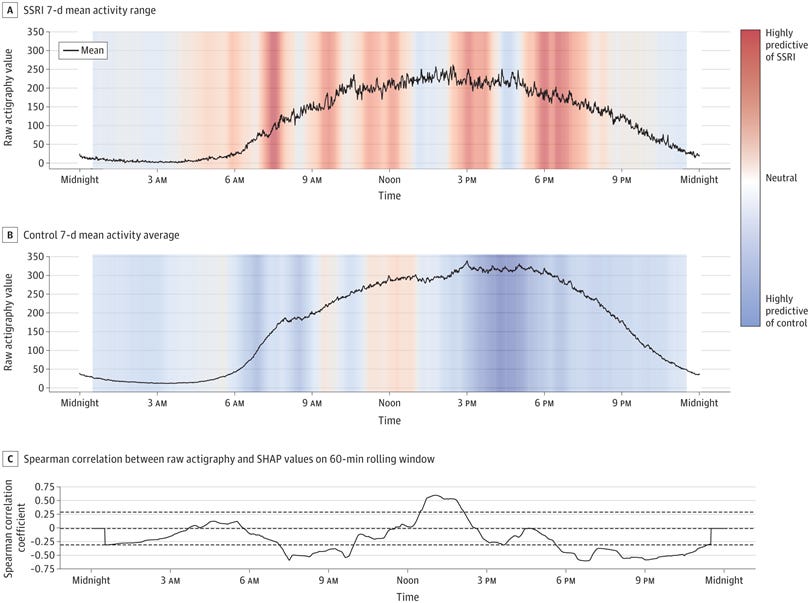
Understanding that depression itself is known to be associated with decreased movement, the researchers used results on the depression screening questionnaire PHQ-9 to compare movement in depressed people who were, and were not, taking SSRIs. Their results held: no matter how depressed people were, they still moved less if they were taking SSRIs.
The authors proposed an explanation for their findings, and set them in the context of the known effectiveness of physical activity in relieving depression:
“The overall decreased intensity of movement in the SSRI group is consistent with the central fatigue hypothesis,12 which emphasizes the importance of monoamine neurotransmitters, such as serotonin and dopamine, in regulating physical activity and fatigue [specifically, increased serotonin in the brain can lead to an earlier onset of fatigue under exertion]. Robust evidence from animal studies suggests decreased performance (ie, shorter time to fatigue) in response to increased serotonergic activity.34 Although similar results have been found in humans,35 the outcomes are more mixed and the evidence less robust.12 This association between SSRI use and overall decreased movement is especially important considering the benefits associated with physical activity and exercise for individuals with mild to moderate depression.36”
Put simply, SSRI antidepressants may undermine the beneficial effects of physical activity on depression by making people feel more tired when they exercise. Good for ongoing sales of the drug; bad for depressed people.
3. The prevalence of sexual dysfunctions and sexually related distress in young women: a cross-sectional survey
This study surveyed almost 7000 Australian women aged 18–39 years to ascertain the prevalence of sexually-related personal distress and female sexual dysfunction. Five domains of female sexual dysfunction were assessed: dysfunctions in desire, arousal, orgasm, responsiveness and sexual self-image.
Shockingly, one in five participants reported having at least one female sexual dysfunction, and fully half of these young Australian women experienced sexually-related personal distress, either with or without an identifiable female sexual dysfunction.
20.5 per cent of participants were taking psychotropic medication (of which SSRIs are the most commonly prescribed), and these drugs had the most pervasive impact on sexual function of any variable studied.
For example, being on a psychotropic medication was associated with more than double the risk of experiencing dysfunctions of sexual desire and arousal, a 48 per cent higher risk of orgasmic dysfunction, a roughly 75 per cent higher risk of dysfunctions of both responsiveness and sexual self-image, and almost double the odds of experiencing nonspecific sexually related personal distress.
Fukitol, indeed.
As the authors of the study point out,
“Sexual well-being is a fundamental human right. That approximately one-half of young women experience sexually related personal distress and one in five women have an FSD, with sexual self-image dysfunction predominating, is concerning.”
You want to know what else is concerning? The fact that prescriptions for psychotropic drugs, especially SSRIs, are handed out like lollipops to this demographic group, with absolutely no regard for the devastating effect that treatment-induced sexual dysfunction has on their well-being, not to mention on their relationships.
Is it just me, or are you starting to wonder whether this is deliberate? Healthy intimate relationships can be a source of tremendous support for people who are going through tough times. Drugs that reduce sexual satisfaction can undermine such relationships, driving distressed young women out of the arms of their lovers and into the waiting clasp of the medical-industrial complex. Again, good for Big Pharma, bad for us.
Speaking of that…
4. Antidepressants produce persistent Gαs associated signaling changes in lipid rafts following drug withdrawal
Not such a catchy title, but this study delved into the reasons why withdrawing from antidepressants is so difficult.
As I discussed in Antidepressant discontinuation syndrome – an underrecognised and rapidly escalating problem, many people experience unpleasant symptoms including insomnia, anxiety, irritability, impaired concentration, headache, lethargy, and low mood, when they stop taking antidepressants. These symptoms are frequently misinterpreted, either by the patient or the prescribing doctor – or both – as a relapse of their depression, causing them to believe that they ‘need’ to take the drug on an ongoing basis in order to function.
In this study, researchers demonstrated that the reason for both the slow onset of action of these drugs (some can take up to two months to exert their activity) and the distressing withdrawal symptoms that they cause, are due to the fact that the drugs collect gradually in cholesterol-rich membrane structures called lipid rafts, affecting the function of a protein called Gαs protein which in turn ramps up the production of an intracellular signalling molecule called cyclic AMP.
When people stop taking antidepressants, lipid raft Gαs signalling is impacted for an extended period of time, causing many of the disturbing withdrawal effects.
There are some differences between individuals in how they metabolise Gαs, and also some differences between antidepressants in how they impact on Gαs signalling, explaining why some people can abruptly stop taking antidepressants without ill effects, whilst others need to be weaned off them very slowly to avoid horrendous withdrawal effects.
5. Individual Differences in Response to Antidepressants: A Meta-analysis of Placebo-Controlled Randomized Clinical Trials
It’s become increasingly clear over the years that antidepressants don’t work any better than placebos (inactive ‘dummy pills’), when pitted against them in randomised, double-blind, placebo-controlled trials.
Never one to give up in the face of comprehensive, repeated failure, however, Big Pharma and its white-coated drug pushers retreated to a new position: Some antidepressants work better for certain people, so doctors should simply try one antidepressant after another on their depressed patients until they find the magic pill that drives their blues away.
And the evidence for that contention? Nada, as the authors of this study point out:
“Despite the paucity of studies designed to detect treatment by individual interactions, there is a widely held assumption that individual differences moderate the effect of antidepressants on depressive symptoms (ie, response).”
And, after conducting a meta-analysis of 91 randomised clinical trials, involving 18 965 participants, on the use of antidepressants in major depression, they concluded that the belief that antidepressant therapy can be personalised based on individual treatment effects is as big a crock of crapola as all the other overblown claims made for these drugs that promised you better life through chemistry.
“Responses to all antidepressant classes were not more variable than responses to placebo”
… meaning that depressed people’s response to placebo showed as much variation as their response to taking any type of antidepressant drug. Whether or not a depressed person feels better when given a pill that they’re told may help them, seems to pretty much depend on how much they believe that the drug will work for them, at that point in time, rather than the ingredients in the pill:
“Data from RCTs [randomised control trials] show that individuals with symptoms of depression assigned to receive the same antidepressant at the same dose and for the same period can experience very different outcomes.5”
And furthermore,
“We found no evidence that the association between treatment group and variability was associated with baseline depression severity.”
Or, in plain English, people with severe depression weren’t any more likely to feel better on any type of antidepressant than on placebo.
Summing up
Antidepressant drugs don’t improve your health-related quality of life, reduce your level of physical activity (which is a key factor in alleviating depression), wreck your sex life and then make you feel like crap on a cracker when you try to stop taking them. And for all that, you’re about as likely to feel better after taking them as you would after taking a placebo. Gee, sign me up now!
But wait, there’s more! I’ve seen an increasing trend towards the prescription of atypical antipsychotics (drugs that were developed to treat severe mental illnesses such as schizophrenia) to people who didn’t feel better for taking antidepressant drugs.
A social worker colleague confirmed my observations, reporting that a concerningly high percentage of her clients – mostly women who are experiencing postnatal depression, but with no evidence of psychosis – have been prescribed drugs like quetiapine (Seroquel), risperidone (Risperdal), aripiprazole (Abilify) and olanzapine (Zyprexa) to “calm them down” or “help them sleep”, when the antidepressants they were prescribed failed to help.
But this study found that adding an atypical antipsychotic to an antidepressant was associated with a 45 per cent increased risk of death compared to adding a second antidepressant (which isn’t any more likely to help with the depression, according to study #5 above).
All this research raises important questions in my mind.
Do doctors know this? If they do, why do they keep prescribing drugs that don’t work, have horrendous side-effects, and could kill their patients? And if they don’t, why not? The onus is on them to ensure that the medications they prescribe are safe and effective, but too many are letting their patients down – in some cases, all the way to the grave.
In my next post, I’m going to summarise several recent articles on the therapies that actually work for depression.
In the mean time, I highly recommend reading A Midwestern Doctor’s excellent series on why most doctors suck so badly at recognising the harm that their treatments inflict on patients, as it’s highly relevant to this topic, and besides that, it’s a damn fine read.
Part 1:
Part 2:
Part 3:
Part 4:




Lots to unpack and comment on, suffice as to say that I agree.
1. Interesting that more women are “depressed” than men. Is it just that blokes are reluctant to seek help ? My mum was probably sad due to loneliness but still enjoyed life.
In days gone by I’d have a few pints with mates after work and a whinge, that was my therapy. These days I still ride to and from work, sedately, but I suspect the exercise is enough to chill emotions and or just give me an emotional boost in.
2. I very much agree with the sentiment that life is full of ups and downs, you can’t always be happy. These days society has become softer.
3. The destruction of the family unit doesn’t help
4. A close family member went through some real bad times, self harm etc. the health dept. was insistent on prescribing some anti- depressants and we reluctantly acquiesced. I will say that they did perhaps take the edge off whatever they were going through, and we were fortunate to find a proper counsellor and a CBT course that resolved their issues. It did need a lot of family support and commitment and not everyone has a supportive family. I’m not sure where I’m going with this, it perhaps reinforcing point 3.
4. Social media doesn’t help. It must put enormous pressure on kids, and interferes with the values and traditions of the family. And now the government is getting in on the act...
While I wrote the post to focus on the COVID vaccines, psychiatric meds are one of the most common medications doctors gaslight their patients with. I know a lot of people who had their lives ruined by them and were typically just told "that's just proof you need the antidepressant." It's very sad to see it happen over and over.