Osteoarthritis: Curse of old age or plague of modernity?
Far from being an inevitable consequence of growing older, osteoarthritis may be the consequence of 'evolutionary mismatch' - ancient genes ill-suited to the modern world.
Osteoarthritis is one of our most common chronic health conditions, afflicting an estimated 2.2 million Australians, or 9.3 per cent of the total population (10 per cent of the female population and 6.1 per cent of the male).
The prevalence of this painful and disabling condition, which is characterised by the breakdown of the cartilage that overlies the ends of bones in joints, increases with age: 22 per cent of those aged over 45, and 36 per cent of those aged 75 and over, suffer from osteoarthritis.
Osteoarthritis is the major diagnosis leading to knee and hip replacement surgery in Australia - and the need for these surgeries is burgeoning. In the decade between 2010–11 and 2020–21, there was a 22 per cent rise in the age-standardised rate of total knee replacement, and a 25 per cent rise in total hip replacement, for people with a principle diagnosis of osteoarthritis:
Most people who develop osteoarthritis are told that it's due to 'wear and tear' - just another one of those cruel punishments dished out by Mother Nature as we get older.
Yet there is very clear evidence that osteoarthritis is far more common now than it was in the past, even after taking our longer average lifespan into account (in fact, knee osteoarthritis is twice as common now as it was in 1950), and that far from being caused by excessive use of our joints (the 'wear and tear' argument), osteoarthritis is aggravated by physical inactivity.
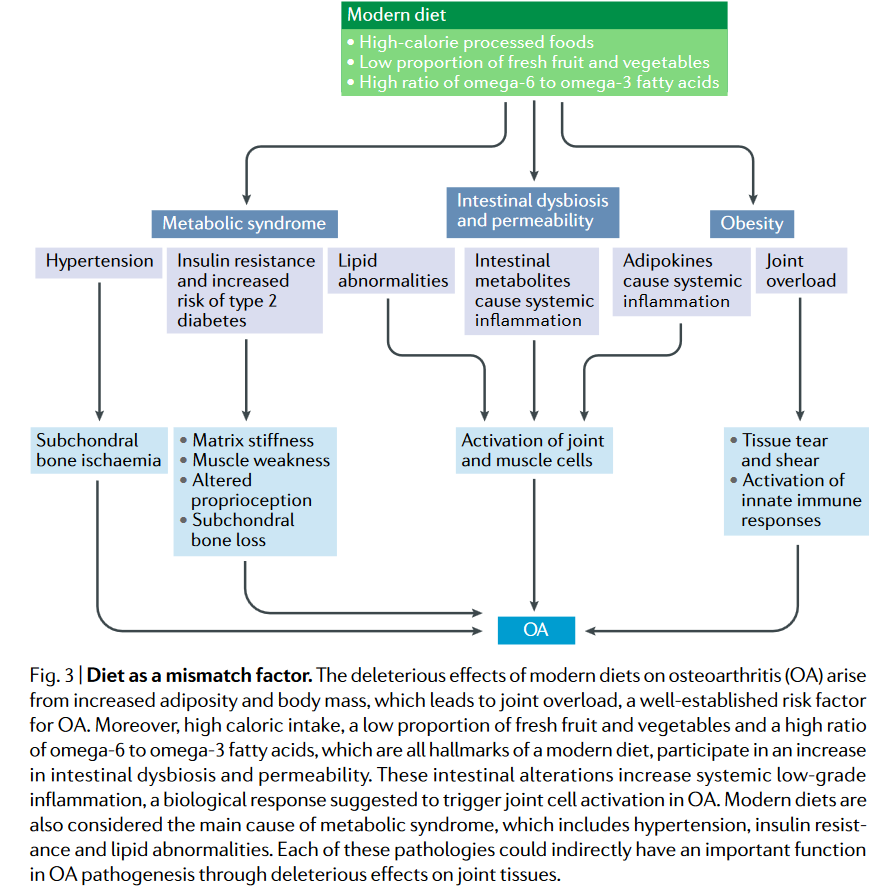
In a highly-readable and well-referenced article titled 'Modern-day environmental factors in the pathogenesis of osteoarthritis', four researchers from France, the UK and US argue that "OA [osteoarthritis] is an evolutionary mismatch disease", and that it is "more common today than in the past because genes inherited from previous generations are inadequately or imperfectly adapted to modern environmental conditions."
Evolutionary mismatch diseases occur when an individual is placed into an environment which is totally different from that in which their ancestors evolved.
Charles Darwin described the mechanism of natural selection as ‘survival of the fittest’, meaning that individuals whose genes are the most well-suited to their environment (i.e. have the best environmental 'fit') are the most likely to survive and reproduce, passing those genes onto the next generation.
Conversely, those whose genes are ill-suited to their current environment are less likely to survive and reproduce, and hence those genes that have a poor environmental 'fit' will gradually disappear from the gene pool of the species.
Over the long course of our evolutionary history, humans developed many adaptations to changes in our environment. For example, as our dark-skinned ancestors gradually dispersed out from equatorial Africa, they developed paler skin that allowed them to make sufficient vitamin D in less sunny climates.
However, rapid changes in a species' environment can outpace the mechanism of natural selection, resulting in a large proportion of that species becoming 'unfit' - that is, suffering impaired health and reproductive capacity because their genes are fundamentally mismatched to their current environment.
Specifically, there are four major drivers of OA that have surged in the last 50 years, and for which the human genome, forged in the unforgiving environment of a food supply that was low in energy density, high in fibre and micronutrient density, and required substantial daily energy expenditure to obtain it, is utterly unprepared:
Obesity;
Metabolic syndrome;
Dietary changes; and
Physical inactivity.
Let's take a deeper dive into each of those four factors.
1. Obesity
Most people know that being overweight or obese increases their risk of developing osteoarthritis, but they usually assume that this occurs because carrying excess weight overloads the joints.
On the contrary, say the authors,
"Loading per se is not bad for joints, as it is necessary for normal joint development and maintenance".
Modern-day environmental factors in the pathogenesis of osteoarthritis
However, when that increased load is combined with malalignment of the knee joint (which can be caused or aggravated by the changes in gait that occur when a person is obese) and muscle weakness, it damages the structure of the cartilage that caps the ends of bones.
In addition, excess body fat releases a slew of chemicals which create a chronic, low-grade inflammatory state known as 'metaflammation'. This metaflammation explains why people who are overfat are more likely to have osteoarthritis in non-weight-bearing regions such as the hands.
2. Metabolic syndrome
Metabolic syndrome, also known as 'syndrome x' and 'insulin resistance syndrome' is a cluster of cardiometabolic factors that commonly accompany obesity, including central adiposity (having a 'spare tyre' of fat around the midsection), dyslipidaemia (high triglycerides and total and LDL cholesterol, with low HDL cholesterol), impaired fasting glucose levels and hypertension (high blood pressure).
In times gone by, metabolic syndrome was practically unknown except among the tiny percentage of the population whose wealth gave them access to its primary driver: excessive and long-term positive energy balance, aka taking in more calories than you expend.
Metabolic syndrome is associated with metaflammation, impaired function of chondrocytes (the cells that produce and maintain cartilage), and accelerated degradation of cartilage.
3. Dietary changes
The energy dense, highly processed modern diet could not be further removed from the low energy-density, high fibre, high fruit and vegetable diet of our forebears.
Multiple elements of the eating pattern characteristic of industrialised nations, and the wealthy in developing countries - including excessive calories, increased ratio of pro-inflammatory omega-6 fatty acids to anti-inflammatory omega-3 polyunsaturated fatty acids, and high sugar, salt and saturated fat content - have been linked with an increased risk of osteoarthritis.
Conversely, multiple elements of a wholefood plant-based eating pattern, which mirrors the diet of our ancestors - including low energy density, and high content of fibre, vitamin K, antioxidants and phytochemicals - have been shown to be protective against osteoarthritis.
4. Physical inactivity
Aside from indirectly contributing to osteoarthritis by promoting obesity and metaflammation, physical inactivity directly increases the risk by reducing biophysical stimuli from the environment which are required to maintain normal joint function:
"Mechanical loads engendered by activity are critical to the development and maintenance of optimal structure and strength of joint tissues and their surrounding muscles."
Modern-day environmental factors in the pathogenesis of osteoarthritis
Your joints obey the 'use it or lose it' principle. If you don't load your joints with regular weight-bearing activity, your cartilage will become thin and defective, making it biochemically vulnerable to the development of osteoarthritis - especially if you suffer an injury or have a joint malalignment.
Contrary to the frequently-expressed concern that weight-bearing exercise such as running may 'wear out' knee and hip joints,
"MRI studies have shown that people who regularly engage in weight-bearing exercise maintain thicker cartilage, and in one study, these individuals were even noted to have fewer cartilage defects, than people who are physically inactive."
Modern-day environmental factors in the pathogenesis of osteoarthritis
NSAIDS - solution to osteoarthritis pain, or part of the problem?
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen are the most commonly-used medications for relief from the pain associated with osteoarthritis. However, in research presented at the 108th Scientific Assembly and Annual Meeting of the Radiological Society of North America in 2022, NSAIDS were not found to have a protective effect on joint inflammation or cartilage thickness in people with moderate to severe osteoarthritis - in fact, quite the opposite.
The researchers recruited 721 participants from the Osteoarthritis Initiative (OAI) cohort, 129 with moderate to severe osteoarthritis and sustained NSAID treatment for at least 1 year, and 592 control participants who did not regularly use NSAIDs.
Each participant underwent MRI scans of their knees at baseline, and then four years later. The participants who took NSAIDs regularly had worse joint inflammation and cartilage quality at baseline than the control group, and both measures of joint health worsened at four-year follow-up compared to the non-NSAID-taking controls.
The lead researcher crisply summarised the findings:
"In this large group of participants, we were able to show that there were no protective mechanisms from NSAIDs in reducing inflammation or slowing down progression of osteoarthritis of the knee joint."
The bottom line:
Most people fear getting older, not least because they equate aging with decreased mobility and increased pain. However, we are not helpless victims of the aging process. And the problems we unthinkingly attribute to getting older do not have pharmaceutical solutions. No one develops osteoarthritis because they have an NSAID deficiency.
Paradoxically, the more we consciously mimic the diet and lifestyle of our ancient forebears by eating a diet centred on foods that are high in fibre, antioxidants and omega 3 fatty acids, and low in saturated fat, omega 6 fatty acids and added salt and sugars, and incorporating weight-bearing and muscle-strengthening exercise into our daily routine, the more benefit we will gain from the increased lifespan that modernity has bestowed upon us. It's a whole new spin on going back to the future!







Spot on, yet again, Robyn!
Loved your sentence: "No one develops osteoarthritis because they have an NSAID deficiency." Ha ha
I have to say, those covid injections seem to have boosted surgery rates, eh? Perhaps one could say that rise is because people were forced to stay at home for a while there by our tyrannical government...but you know, they could've still done exercise at home, gardening; all that sort of stuff. They weren't glued to the lounge! No, they took poison, and now we're seeing the results of that.
I'm also pretty sure the rate of OA is has been GROSSLY underestimated. The link you put in there says that "1 in 5 Australians (22%) over the age of 45 have osteoarthritis" - but as a Country Chiropractor for many years, I saw a lot of patients, and a lot of X-rays, and almost EVERYONE over the age of 25 had OA to at least some degree, in some area/s of their body. And I wouldn't say it was much different between male or female. I wonder how they determine what OA is to get to an average of "9.3%" - does it have to be diagnosed by a GP or something, and drugs prescribed? Because if we're looking at ALL sections of the human body, I'd say about 90% of people over 25 have it! It might be vertebral OA, hip joint OA, sacro-iliac joint OA, let alone the peripheral joint OA (knees, thumbs, shoulders etc). Even in those who didn't have pain in a particular place, the OA there still showed up on X-rays as an incidental finding. So I think the Australian Government has VERY little idea - or care - about what ailments their constituents suffer from.
So many of my country patients also took NSAIDS to help with random pains that came up in their day-to-day lives, or when they injured themselves. I mean, what, paracetamol wasn't good enough (for the social compliance/not caring thing)? Drinking heaps of water was too hard? Listening to me about how to do things right was too hard?! Evidently all that was too hard, because swallowing a pill was a whole lot easier for them. About 95% of them got jabbed, too, so really, I was wasting my time trying to keep people ALIGNED, which is a much better way to stave off OA - even though plenty were overweight/obese, too! But given people's seeming addiction to bad lifestyle choices, it's not exactly rocket science to figure out that things in the body don't tend to STAY aligned when you're doing the wrong things for yourself day in, day out...
I very much enjoy your articles! I have shared your piece on Osteoporosis with many of my patients concerned about ONJ associated with the injectable osteoclast inhibitors.
I am curious your thoughts and any research on the role of absorbed fluoride over the course of a lifetime. I have read that it is implicated in osteoarthritis as it accumulates in the joints. It could also be implicated in metabolic disorders as fluoride in the stomach may contribute to leaky gut.
I am a classically trained dentist and only recently became aware of the dark, dark history of fluoride. Very curious your thoughts!