Antinutrient villain or bone health superhero? The secret life of phytate.
Maligned as a mineral-sapping antinutrient for decades, it turns out that phytate is good to the bone.
Recently, a friend reached out for advice after suffering a wrist fracture. She is very health-conscious and had already been doing the single most important thing that one can do to prevent osteosarcopenia - low bone mass and micro-architectural deterioration of bone, combined with loss of muscle mass, strength and function - namely, weight training. But my friend's wrist took the brunt of a hard fall, and she suffered a Colles fracture, in which the broken end of the radius bone tilts upward:
As the online radiology resource Radiopaedia explains,
"Colles fractures are very common extra-articular fractures of the distal radius that occur as the result of a fall onto an outstretched hand... Colles fractures are the most common type of distal radial fracture and are seen in all adult age groups and demographics. They are particularly common in patients with osteoporosis, and as such, they are most frequently seen in elderly women."
The bottom line is that any bone will fracture if enough force is applied to it, but my friend is in a particularly high-risk category due to her age, sex and build. (She's the second in as many years of my female friends in the 50-plus age group to suffer a wrist fracture which required surgery.) She is recovering well from the surgery, thank goodness, but wanted to know if there's anything she should be adding to her regimen, to reduce the risk of another fracture.

I've written previously about The top 5 tips for building strong, healthy bones and the importance of hitting the sweet spot for calcium intake (not too little, not too much - excessive calcium intake kills off osteoblasts, the cells that build new bone), but there's one important bone health-promoting dietary component that I've never dedicated an article to - phytate.
Yes, phytate, which hordes of ill-informed 'health influencers' histrionically hyperventilate about online, maligning it as an 'anti-nutrient' that you must take pains to minimise, or preferably avoid altogether, lest it steal away your minerals... and maybe even sap and impurify your precious bodily fluids.
But, contrary to the anti-phytate hysteria, it turns out that phytate is good to the bone - unlike George Thorogood.
God, I miss the 80s...
OK, enough messing around. Let's dive into the research on phytate, with a particular focus on its effects on bone.
What the heck is phytate, anyway?
Phytate - also known as phytic acid and myo-inositol hexaphosphate - is the principal storage form of phosphorus in legumes, grains and oil-rich seeds. Phosphorus is a mineral that is essential for both plants and animals. Dietary phytate is absorbed through the gut wall, distributed through body tissues and fluids at levels reflecting intake, and excreted in urine.
Because phytate binds tightly to other essential minerals and trace elements, including calcium, magnesium, iron and zinc, and because monogastric (single-stomached) animals including humans don't produce much phytase (a phytate-degrading enzyme), phytate was long thought of as an anti-nutrient that increased the risk of nutritional deficiencies. There's certainly evidence that zinc deficiency is very common in people with limited diets that rely excessively on unleavened breads such as tanok, lavosh, abud, shrak and chapati. However, the high phytic acid content of unleavened bread is not the only contributing factor; the soils of many of the countries which make heavy use of unleavened breads - including India, Pakistan, Iran and Turkey - are known to be deficient in zinc.
More recent research conducted in populations with greater dietary diversity, has found that a high dietary intake of phytate is associated with a plethora of health benefits including decreased inflammation and pathological calcification within the vasculature and kidneys, improved lipid profile and blood glucose regulation, protection against cancer and - most relevant to the topic of this post - decreased age-associated bone mass loss:

Importantly, phytate both reduces bone loss AND stimulates the formation of new bone - a double-act unmatched by osteoporosis drugs, which decrease the breakdown of old bone while inhibiting the formation of new bone by up to 95 per cent. I'll get to the mechanisms by which dietary phytate enhances bone health in a tick, but first let's survey the evidence from population studies and one intervention trial.
Epidemiological studies linking high phytate intake with bone health
Dissing epidemiological or observational research is a popular sport among many self-styled nutrition dissidents. Whenever such a study is published that contradicts their preferred narrative, you'll hear the battle cry go up: 'Correlation isn't causation!' Yeah, no sh*t, Sherlock. No one in the research world ever said it was. The primary purpose of both cross-sectional (single time-point) studies and cohort studies (in which the occurrence of a particular disease is tracked over time in a defined population with varying levels of exposure to suspected risk factors for that disease) is to generate hypotheses about causality, not to prove it. The observations drawn from epidemiological research are then explored in laboratory research, to identify mechanisms that could explain how the exposure might cause the observed effect, while intervention studies turn the exposure into a treatment which can be applied to people who already have, or are at high risk of developing, the disease, to see if there is indeed a causal relationship.
Having said all that, if multiple epidemiological studies conducted by different research teams in widely varying populations, in many different locations, all come out with similar findings, and most particularly if there is a dose-response relationship between the exposure and disease (for example, if people who smoke three packs of cigarettes per day have a higher rate of lung cancer than people who smoke half a pack) and if there is an established mechanism of action, then we can more confidently assume a causal relationship, according to the Bradford Hill criteria of causality.
So what evidence do we have, that people with a higher dietary intake of phytate, have better bone health?
A 2008 study measured the calcaneal (heel) bone mineral density (BMD) of 1473 adults aged 18-65, and the lumbar column and femoral neck BMD of a subset of 433 of them. BMD was significantly higher at each location in participants who ate phytate-rich foods at least three times per week, than in those who ate less than three servings per week.
The same research team followed up with a study of postmenopausal women, published in 2013, which measured both BMD in the lumbar spine and femoral neck, and urinary phytate concentration, at baseline and at 12-month follow-up. Women with a higher urinary phytate concentration had higher BMD in both locations at baseline. Among women who remained in the same bracket of urinary phytate excretion (low, intermediate or high) at follow-up as they had been at baseline, a significantly higher percentage of those with persistently low urinary phytate lost more than two per cent of their lumbar and femoral neck BMD at follow-up. Conversely, those with persistently high urinary phytate were more likely to have lost less than two per cent of their bone density at follow-up. The 10-year probability of both hip and major osteoporotic fractures (calculated using the FRAX tool, which takes into account both bone mineral density and other risk factors for fracture) was also significantly higher in the low-phytate group compared to the high-phytate group.

In a 2019 study of postmenopausal women, those with low urinary phytate concentration (indicating low dietary intake) had a higher risk of hip and major osteoporotic fracture than women with high urinary phytate excretion, as calculated by the FRAX model.
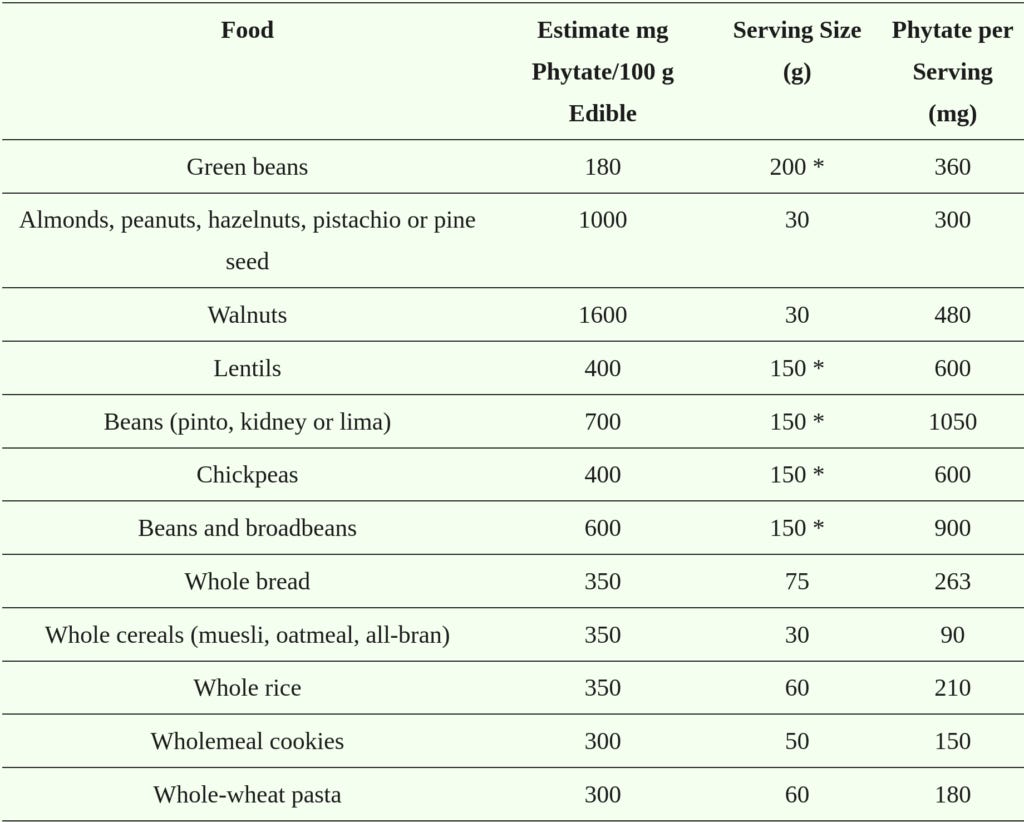
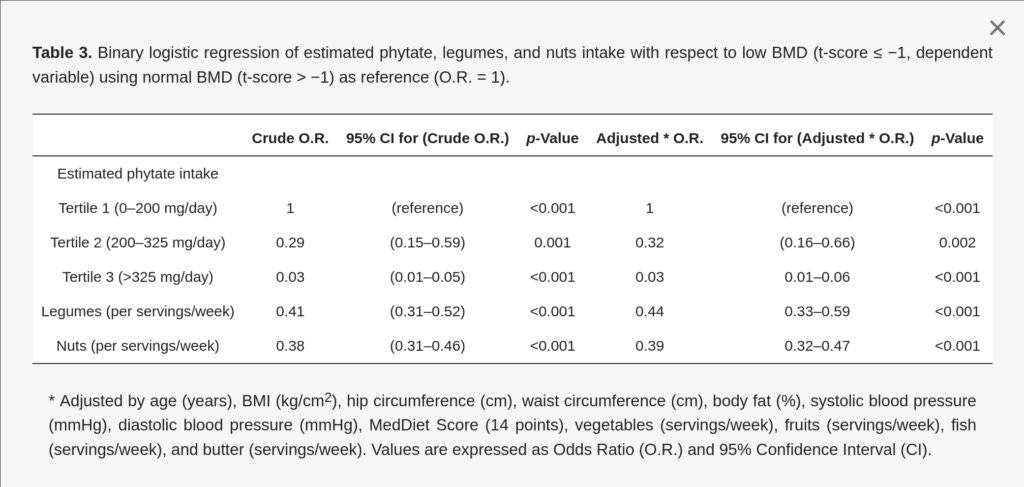
Another study of postmenopausal women, published in 2021, found an inverse relationship between phytate intake bracket and both BMD and T-score (the difference between the subject's BMD and that of a young adult) - that is, the higher the dietary phytate intake, the higher the bone density. Similarly, intakes of phytate-rich legumes and nuts were both inversely associated with BMD. The odds of having low BMD were lowest in women consuming more than 325 mg of phytate per day. A single serving of legumes or nuts contains between 300 and 900 mg of phytate, so just one serving per day might be enough to hit the phytate target.
A study published in 2023 analysed femoral and lumbar spine BMD in a subset of overweight postmenopausal women with metabolic syndrome, from the PREvención con DIeta MEDiterránea Plus (PREDIMED-Plus) trial, in relation to the women's dietary phytate intake. Women in the top tertile of phytate intake had higher BMD values and T-scores in almost all the individual sites measured in both the lumbar spine and femur, even after adjusting for potential confounding factors including age, BMI, physical activity level, educational level, smoking status, type 2 diabetes prevalence, osteoporotic fractures prevalence, dietary glycaemic index, and intake of energy, calcium, vitamin D, vegetables and fruits. Those who had normal BMD (T-score greater than −1) were also more likely to have a higher phytate intake than those with low BMD (T-score less than −1).
So far, the findings from published epidemiological studies have been extremely consistent: high intake of phytates, measured either via food frequency questionnaires or urinary excretion, are associated with higher bone density, a lower risk of abnormally low bone density, and decreased calculated fracture risk.
There are a few caveats and important considerations to point out:
Publication bias. Studies that fail to find a statistically significant result are less likely to be published than those that do, either because the researchers don't want to publish them, or because journals decline them because they're not as likely to be read, which decreases the journal's impact factor (the rough equivalent of ratings for TV shows). Australia and New Zealand, the US, the European Union, and the World Health Organisation all run registers for clinical trials (i.e. studies in which a treatment is being investigated) in an attempt to minimise non-publication - an attempt which appears to be failing - but no such registers exist for non-clinical research. Is it possible that some studies which found that phytate intake had a negative effect on bone density, or no effect at all, remain unpublished? Yes, it is possible, but unlikely given the established mechanisms of action of phytate on bone, which we'll get to shortly.
Confounding. Confounding occurs when an independent risk influences the relationship between the risk factor being studied, and the outcome. For example, influenza vaccine efficacy studies are confounded by the fact that people who are at the lowest risk of suffering lethal complications from the flu are more likely to get the flu vaccine than those at highest risk. Although all epidemiology researchers apply statistical adjustments to correct for known confounds such as age, activity level and overall dietary pattern, no correction is perfect, and there may also be unknown confounding factors. In the case of the phytate-bone health studies, confounding shades into...
Reductionism. Most scientific research is reductionist by its very nature, as researchers must pick something to focus on, and grant funding favours an extremely narrow focus. It's important to note that diets that are high in phytate (but are not dependent on a single food, particularly unleavened bread) are, necessarily, rich in legumes, whole grains, nuts and seeds - foods that contain a plethora of bioactive constituents with already-established benefits for human health, including bone health - and that conversely, they will be lower in less-healthy foods. For example, in the PREDIMED-Plus cohort,
"Women in the highest tertile of phytate intake had higher physical activity and a lower glycemic index than those in the lowest tertile. Regarding food intake, women in the top tertile consumed more vegetables, legumes and nuts and less meat, olive oil and pastries and sweets when compared to the lowest tertile."
Surrogate measures. All the epidemiological studies listed above use surrogate measures of bone health - primarily bone mineral density as measured using dual-energy X-ray absorptiometry (DXA) scanning, and/or the FRAX tool which utilises known risk factors for fracture, with or without DXA results. I have written at length about the serious limitations of BMD screening of healthy people, and the validity of the T-scores that emerge from it. It would be nice to have some cohort studies which tracked actual fractures over time, but such studies would require large numbers of participants and long follow-ups, which means they need major funding.
Given all this, how can you be sure that eating more phytate-rich foods will help you have stronger, healthier bones? Let's look at...
Clinical trial evidence that phytate improves bone health markers
The first randomised pilot study on the effects of daily phytate supplementation on BMD was published in 2022. 23 patients with hypercalciuria (elevated calcium loss via the urine) and kidney stones secondary to bone resorption, who had a BMD indicating either spinal and/or femoral neck osteopenia or osteoporosis, and a ß-Crosslaps level greater than 0.4 ng/mL (indicating accelerated bone breakdown) were randomised to receive either 380 mg of calcium-magnesium inositol hexakisphosphate per day, or no treatment. After three months, patients receiving phytate supplementation had a significantly lower 24 hour urinary calcium level than controls. Despite randomisation, the phytate group began the study with a much higher ß-Crosslaps level than controls, indicating that their bones were undergoing more rapid resorption. Their ß-Crosslaps level dropped by almost 30 per cent after three months of phytate supplementation, while the controls' ß-Crosslaps level did not change:
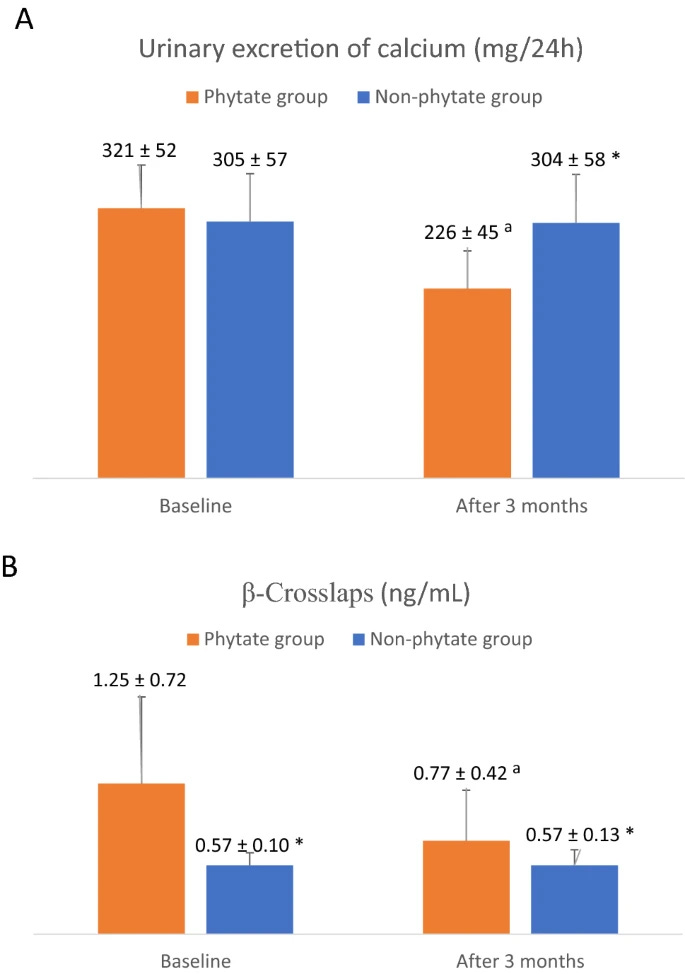
ß-CrossLaps, also known as C-telopeptide cross-linked type I collagen or beta-CTx, is a biomarker of bone resorption - the process of breaking down old, damaged, or defective bone. The test is used to monitor the impact of antiresorptive therapies including bisphosphonates and hormone replacement therapy, in people undergoing treatment for osteoporosis and osteopenia. Here's how an adequate therapeutic response is defined:
"In patients taking antiresorptive agents (bisphosphonates or hormone replacement therapy), a decrease of 25% or more from baseline beta-CTx levels (ie, prior to the start of therapy) 3 to 6 months after initiation of therapy indicates an adequate therapeutic response."
Remember, after three months of phytate supplementation, ß-CrossLaps/beta-CTx levels dropped by almost 30 per cent, comparing extremely favourably to pharmaceutical antiresorptive therapies.
Again, plenty of caveats apply: It was a small study, involving relatively young people with kidney stones related to idiopathic bone resorption, rather than the standard pattern of age-related bone density loss. Although there is some overlap between the pathogenesis of kidney stones and osteoporosis, only a clinical trial enrolling postmenopausal women and older men at high risk of osteoporotic fracture, will tell us whether phytate is as effective for preserving bone health in these demographics. But there's reason for optimism given the established mechanisms of action of phytate, which we'll (finally!!!) dig into, now.
Phytate's effects on bone remodelling
Bone remodelling is the process of resorption of old bone, with its accumulated defects from daily use, and its replacement with new bone. It occurs continuously over the lifetime of an individual, in order to facilitate skeletal growth, repair damage (both subclinical, i.e. microfractures, and clinically-evident fractures) and adapt bones to patterns of use (e.g. the thickening of bones in the dominant arm of tennis players). During our youth, the deposition of new bone exceeds the resorption of old bone. As we get older, more old bone is resorbed than new bone is laid down, such that bone mineral density (BMD) declines with age.
Resorption of old bone by osteoclasts is actually necessary for osteoblasts to build new bone. Osteoclasts are modified immune cells that secrete acid and a collagen-digesting enzyme to break down old bone. Osteoblasts, which arise from mesenchymal stem cells, secrete bone matrix constructed from dense crystals of hydroxyapatite (a calcium phosphate compound) into the spaces left by the osteoclasts.
Phytate and bone resorption
The most widely used drugs prescribed for pathologically-low BMD are the bisphosphonates - drugs such as Fosamax, Actonel, Didrocal and Aclasta. I've discussed the limitations and adverse effects of these agents in a previous article, Osteoporosis drugs: Not all they're cracked up to be, so don't assume I'm a fan of these drugs. However, what's relevant to our present discussion is that bisphosphonates work by inhibiting the resorption of bone by osteoclasts.
Specifically, bisphosphonates attach to the hydroxyapatite binding sites on bony surfaces that are undergoing active resorption, and prevent osteoclasts from releasing acid to dissolve the hydroxyapatite. Bisphosphonates also decrease the development of new osteoclasts from their progenitor cells.
And guess what - so does phytate! That shouldn't surprise you too much, once you realise that bisphosphonates are a synthetic analogue of pyrophosphate, a phosphorus compound produced by the body to regulate bone mineralisation, and that phytate (which, as you'll hopefully remember, is a phosphorus storage compound) has overlapping activities with pyrophosphate.
Like bisphosphonates, phytate adsorbs (forms a film on) calcium crystal surfaces, preventing their dissolution. It also reduces the activities of osteoclasts, thereby protecting against bone resorption.
Remarkably,
"Phytate can inhibit hydroxyapatite dissolution in a concentration-dependent manner, similar to alendronate [Fosamax] and to a greater extent than etidronate [Didronel]."
Phytate (myo-Inositol Hexaphosphate) and Risk Factors for Osteoporosis
The following figure shows the concentration-dependent inhibition of dissolution of hydroxyapatite crystals by acid, when the hydroxyapatite was pre-treated with phytate, alendronate or etidronate:
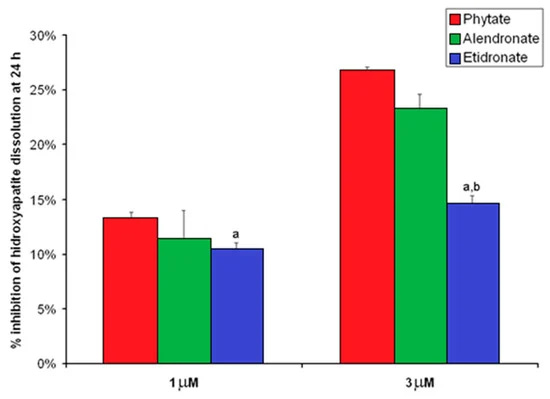
While this is an in vitro study, the implications are intriguing: if hydroxyapatite crystals within bone are constantly bathing in a phytate-rich environment, their dissolution by the acid secreted by osteoclasts will be inhibited. The physiological concentration of phytate in blood plasma has been reported to be 0.4 μM under a 'normal' diet, suggesting that achieving the intake of dietary phytate we'd need to consume in order to reach the concentration of phytate that demonstrated maximum inhibition of hydroxyapatite dissolution would be rather challenging. On the other hand, in the same study that compared phytate to bisphosphonates, the authors found that the consumption of more than 307 mg of phytate per day was associated with a normal bone mineral density in postmenopausal women.
All this is pretty cool, but there's a problem: As I mentioned before, the dissolution of old bone by osteoclasts is necessary for new bone to be built by osteoblasts. The horrific adverse effects of long-term use of bisphosphonates are directly attributable to excessive inhibition of osteoclast activity combined with a decrease in osteoblast activity, which results in the retention of weakened bone rather than the construction of healthy, resilient new bone. So wouldn't it be amazing if phytate helped with the building of new, healthy bone? Oh, wait...
Phytate and bone formation
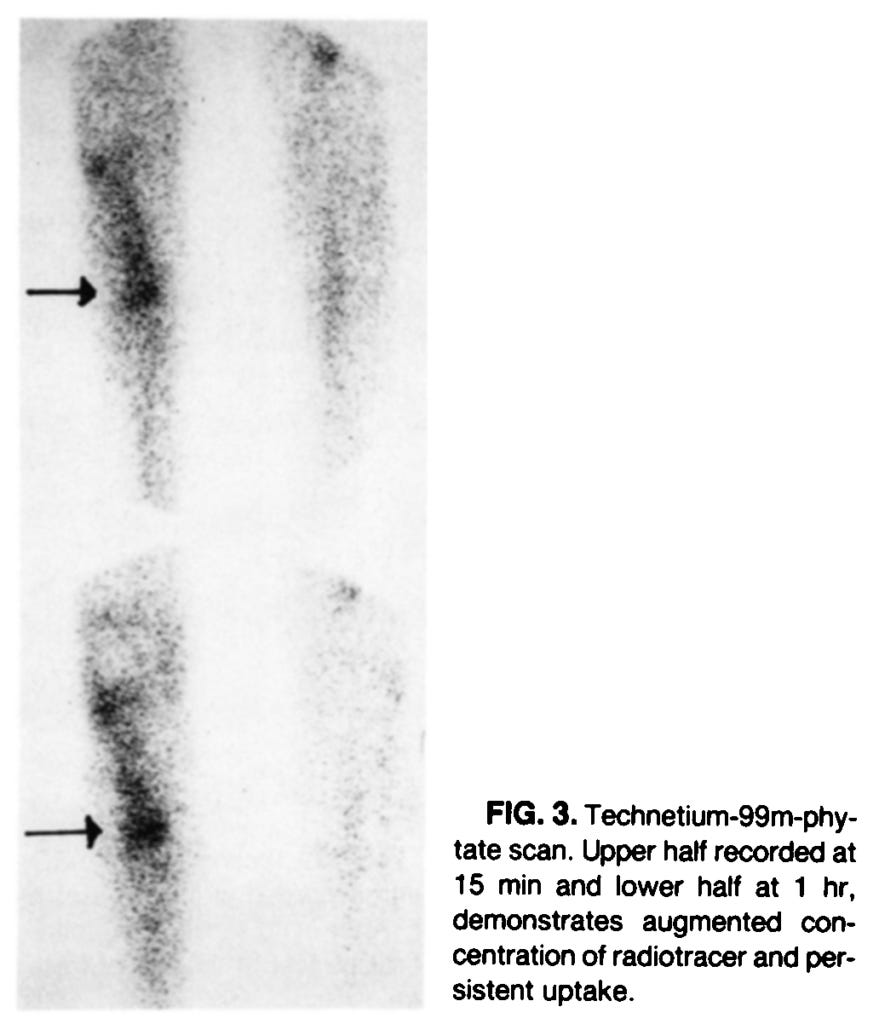
Back in 1990, Indian researchers discovered that when technetium-99m-phytate, a sodium phytate compound to which the radioactive element technetium is bound, is injected into people who have suffered bone fractures, it becomes concentrated at the site of the healing fracture:
This intriguing finding, which implies that phytate is avidly taken up by cells engaged in bone repair, seems to have been largely ignored for decades... until 2021, when Chinese researchers showed that coating titanium with a calcium phytate compound accelerated osseointegration - the formation of a direct structural and functional connection between living bone and the loading surface of an implant. This finding has obvious implications for dental implants, which utilise titanium screws that must fuse with the jawbone in order to be successful. Inadequate osseointegration is one of the principal reasons for implant failure, so anything that enhances osseointegration is great news for dental implant patients - especially if it's as benign a substance as phytate!
But there's another important implication: osseointegration closely resembles fracture healing, and for fracture healing to occur, osteoblasts must be recruited to build new bone. This wasn't lost on the lead author of the titanium osseointegration study, Chunbo Tang. Tang followed up with a 2023 study which elucidated the mechanism by which calcium phytate induced bone regeneration in a rat model. And Tang then coauthored two papers published earlier this year, which demonstrated that in vitro, phytate improves the formation of new bone (osteogenesis) in a high-glucose environment, induces more bone marrow mesenchymal stem cells (BMSCs) to differentiate into bone-building osteoblasts, and prevents the senescence (aging-related decline in health and function) of the BMSCs.
Why test the effects of phytate in a high-glucose environment? Because diabetics have an increased risk of fracture and delayed bone healing, due to decreased BMD, abnormal bone microstructure, and weakened osteogenic function - all of which is downstream of high-glucose conditions:
"A high-glucose environment caused by diabetes can inhibit BMSC proliferation, migration, and osteogenic differentiation [8,9]. In this context, the reactive oxygen species (ROS) production also increases, leading to oxidative stress, which in turn accelerates BMSC senescence [10,11]. Therefore, hyperglycaemia is an inevitable barrier to stem cell-mediated regeneration [12]."
It's been known for many years that phytate has potent antioxidant activity, reduces HbA1c (a marker of average blood glucose level) and beneficially affects levels of leptin and adiponectin which are deranged in diabetics. But the ability of phytate to overcome the inhibitory effect of hyperglycaemia on new bone formation is an exciting new finding. It remains to be confirmed in interventional studies, but while we wait for those to be performed, I don't see any downside to recommending higher intake of phytate-rich foods to people with diabetes, prediabetes and metabolic syndrome, especially if they have additional risk factors for fracture such as postmenopausal status.
And of course, Tang's discovery does not only apply to people with impaired blood glucose control. The protection of BMSCs against senescence, and the funnelling of more BMSCs down the pathway to differentiating into bone-building osteoblasts, is relevant to everyone who is experiencing, or is at risk of, bone loss related to aging or disease processes.
Unlike the bisphosphonate drugs, which restrain bone resorption but also inhibit the formation of new bone, leading ultimately to higher bone density but lower bone quality, it appears that phytate may offer us the best of both worlds. And isn't it deliciously ironic that the very substance that both tamps down excessive bone loss and revs up bone-building, has been maligned as a bone-sapping 'antinutrient' for decades? I think so 🤣.
P.S. Here is a handy-dandy chart summarising the phytate content of some commonly-eaten foods. Dig in!




Outstanding article! Thank you for the time you take to educate us on complicated topics to help us live healthier lives. I will feel even better about my daily dose of almonds and/or walnuts. Thanks for highlighting your past articles on this topic as well. You are a true gift to the world of healthy living!!
You know the reason I like what you do is, at some point after citing multiple studies, you get down to what has become my favorite phrase; mechanism of action. What do you think the phytate poo-pooers say is the mechanism of action for why phytates should be avoided? Additionally, is there really a concern over anti-nutrients, e.g., lectins? Finally, I’ve read that for those who eat red meat, which is high in phosphorus, they should increase calcium intake to neutralize it. I know you’ll probably say don’t eat red meat, but…